INTRODUCTION
Periodontitis and peri-implantitis are both caused by the host’s immune response to specific microorganisms. Mechanical debridement is currently the gold standard treatment for periodontitis, but systemic antibiotics are also prescribed for deep pockets, furcation areas, inaccessible areas, and persistent infections. Furthermore, antibiotics are widely used to prevent postoperative infection after surgical periodontal treatment, to treat acute periodontal conditions, and to prevent infection. However, studies have shown that using systemic antibiotics in addition to mechanical periodontal therapy provides statistically significant benefits. Systemic antibiotics have been linked to reduced pocket depth and better clinical outcomes in patients with stage 3–4 periodontitis1-5.
Antibiotic use is a common concept in periodontal treatment choices to prevent postoperative infections6-8. The value of rapid and inexpensive application of antimicrobial agents to enhance the effects of mechanical periodontal debridement and surgical treatment is remarkable. Patients with periodontal problems may benefit from systemic medications, topical antibiotics, and topical antiseptics. There is a debate about the usefulness of topical antibiotics in periodontal therapy. However, therapeutic success or failure is determined not only by chemotherapeutics’ intrinsic antimicrobial activity but also by the patient’s clinical condition, the location of the subgingival calculus and infection (furcation/deep periodontal pockets)1. Systemic antibiotics enter the periodontal tissues with blood and serum and affect organisms that cannot be removed by mechanical treatment and topical antimicrobials. It also delays subgingival colonization by suppressing periodontal pathogens localized on the tongue or other oral regions9.
Periodontists have difficulties prescribing antibiotics for periodontal surgery. In this case, dentists try to evaluate the need for antibiotics with the guidelines or their personal experiences, and this confusion could lead to antibiotic resistance, antibiotic-related hypersensitivity, ineffectiveness, and suprainfection10. Numerous studies have determined that antibiotic prophylaxis in surgical or non-surgical periodontal treatments is beneficial in the prevention of infection3-6,10,11.
It is a known fact that there is a mutualistic balance between the endogenous bacteria and the host-immune system. Even a single dose of antibiotics can reduce antimicrobial peptide secretion and cause changes in the number of T-helper cells, thus increasing the likelihood of the patient developing an infection12. Although these effects are typically transient, they impact the gut microbiome, which is vital to the host immune response, and this effect may be permanent13,14. In this process, changes in chemotaxis, differentiations in lymphocyte transformation, a decrease in phagocytosis activity, bone marrow suppression and a decrease in antibody production may occur15.
A systematic review stated that using antibiotics as adjunct to periodontal treatment increased the attachment level but did not make a significant clinical difference in periodontal surgery16. In studies investigating the efficacy of antibiotics in osseous surgery, no benefit was found, and infection was developed in some prescribed antibiotics patients17,18. The low incidence of infection in periodontal treatments and unconfirmed antibiotic prescriptions that may cause potential harm to patients, have revealed the necessity of investigating the suitability of systemic antibiotics in periodontal treatments. The German Society of Periodontology published a guideline on adjuvant systemic administration of antibiotics for subgingival instrumentation in the context of systematic periodontitis treatment in 201819. This guideline is very recent, conducted with high methodological standards, and has similar results to EFP clinical practice guidelines1. Survey studies in dentistry are not a new research method, but these can be used to determine the tendency and preferences of physicians to prescribe antibiotics. Therefore, the present study aimed to evaluate the timing and preferences of periodontists in prescribing antibiotics as adjunct to periodontal treatments and implant surgery.
METHODS
Study design, setting and participants
This study involved a mailed survey of 450 periodontists in clinical practice in a university or private clinic in Turkey; 108 respondents answered the survey completely (response rate 25.16%), conducted in March–July 2020. The survey was mailed to the institutional e-mails of periodontology specialists and periodontology residency students, and reminder e-mails were sent to the participants after a week (https://docs.google.com/forms/d/1Y8irW8ltCLh_OGDSHu76CmcuTCXzAyDgQFS9sCJs7NA/edit?ts=611fb4d1).
The study protocol was approved by the Bolu Abant Izzet Baysal University Medical Faculty’s Ethics Committee (Approval date: 16.07.2019; Number: 2019/183). Participants gave their consent for the processing of personal data according to the “Turkey Data Protection Rule”. The survey was accomplished with no identification of any participants.
Questionnaire design and analysis
The survey was designed to investigate the current trends in prescribing systemic antibiotics for the treatment of periodontal and peri-implant conditions by periodontists in Turkey. The layout consisted of straightforward questions with multiple tick-box responses. The survey only asked specific, closed-ended questions; not all of them had to be answered. Respondents were directed to another question based on their responses. Furthermore, participants were asked to complete the survey while keeping in mind that the patients were systemically healthy and did not have antibiotic allergies, and the females were not pregnant or lactating.
Before the data collection, the questions were checked by 10 periodontists who did not take part in the study. The questions were controlled for clarity and comprehensibility. Inter-rater validity coefficient was satisfactory (r=0.35, p<0.05). According to their feedback, some questions were modified to avoid misunderstandings. Demographic characteristics of the participants and their use of systemic antibiotics and their type, dose and timing were evaluated by questionnaire. In addition, we sought to differentiate the prescription choice of antimicrobials in surgical and non-surgical periodontal therapy.
The total number and percentages of respondents were calculated for each question. The descriptive statistics were undertaken using the SPSS 23.0 (IBM corp., Chicago, IL, USA).
RESULTS
Demographic data
Of the 108 respondents who participated in this study, 69 (63.9%) were female and 39 (36.1%) were male periodontists; 50% of the participants were aged 30–39 years and 40.7% 20–29 years. The majority (73.1%), reported that they are currently working at a university. The demographic data of the individuals included in the study are shown in Table 1.
Table 1
The demographic data of the individuals (N=108)
Use of systemic antibiotics in non-surgical periodontal therapy
The majority of participants (71.3%) had received education about systemic antibiotic use and/or prescribing in the last 2 years. Among those that had received education, 38.7% received it from congress/seminars/panels, and 38.7% from the Faculty of Dentistry.
When the use of antibiotics as adjunct to the non-surgical periodontal treatment was assessed, 55.6% of the participants stated that they have prescribed antibiotics in addition to this treatment. Amoxicillin Clavulanic Acid (AMC) + Metronidazole (ME) was the most common choice (48.3%) of antibiotic, followed by Amoxicillin (AM) + Metronidazole (ME) (18.3%). With regard to the timing of the prescription, 45% responded:
‘I complete the non-surgical periodontal treatment and then prescribe it and start using it immediately (only after the treatment)’.
The second most common choice was:
‘I prescribe only before non-surgical periodontal treatment and start using it before treatment, I do not continue using it during and after treatment.’
Of the 16 participants who thought that systemic antibiotics should be prescribed both before and after non-surgical periodontal treatment, 43.8% chose the combination of AMC 625 mg + ME 500 mg and 31.3% used the combination of AMC 1 g + ME 500 mg. The 32.6% of 46 participants who found it appropriate to prescribe systemic antibiotics only for post-treatment process for non-surgical periodontal treatment, reported that they would prescribe a combination of AMC 625 mg + ME 500 mg, and 28.3% would prescribe the combination of AMC 1 g + ME 500 mg. All participants’ responses regarding the prescription of antibiotics in non-surgical periodontal therapy are shown in Table 2.
Table 2
Questions and responses of participants regarding non-surgical periodontal therapy
Use of systemic antibiotics in surgical periodontal therapy
Systemic antibiotics were used by 77.8% (84 participants) of periodontists for surgical periodontal therapy. The most frequently prescribed was the combination of AMC (63.1%) and AMC + ME (27.4%). The remaining participants prescribed other antibiotic derivatives, which are detailed in Table 3. When the timing of antibiotic prescribing was evaluated, 66.7% prescribed medications after the completion of the surgical treatment, 29.8% both before and after the surgery, and 3.6% only before the surgical treatment.
Table 3
Questions and responses of participants to surgical periodontal therapy
Of the group that prescribed antibiotics only before treatment, 66.3% noted that they prescribed medication 1 hour before the procedure, and 33.3% 1/2/3 days before the procedure. When the prescribing details of the same group were examined, it was determined that they prescribed AM 2 g (33.3%), AMC 625 mg + ME 500 mg (33.3%), and AMC 2 g (33.3%). When the group who prescribed antibiotics both before and after the surgical treatment were examined, the responses were Azithromycin 500 mg (44%), AMC 1 g + ME 500 mg (20%), AMC 625 mg (16%). The responses of the group who prescribed antibiotics only after surgical treatment were evaluated, it was observed that AMC 1 g (50%) and AMC 625 mg (19.6%) were the most frequent answers against this situation (Table 3).
Use of systemic antibiotics for pain, fever and lymphadenopathy
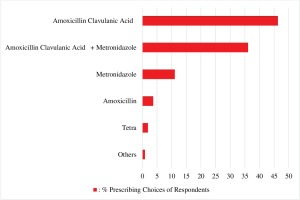
All participants stated that they prescribed antibiotics in the treatment of acute periodontal or gingival conditions accompanied by systemic symptoms such as pain, fever, lymphadenopathy; 46.3% of the respondents stated that they prescribed AMC, 36.1% AMC + ME and 11.1% only ME. The answers given by the other participants are shown in Figure 1.
Use of systemic antibiotics in implant surgery
The preferences of the participants to prescribe antibiotics for the conditions that may occur in the treatment of periimplantitis were also evaluated. The participants stated that they would prescribe antibiotics in cases such as the presence of suppuration (44.4%), probing pocket depth greater than 5 mm (7.4%), and radiographic marginal bone loss greater than 2 mm (2.8%) (Figure 2 A). In the presence of peri-implant abscess accompanied by systemic symptoms, 87% of the participants declared that they would prescribe antibiotics (Figure 2 A). When the antibiotic combinations that the same individuals would prefer in the treatment of peri-implantitis were examined, the majority (56.5%) preferred AMC + ME, and 33.3% only AMC (Figure 2 B). The systemic antibiotic prescribing times of the same group in surgical procedures such as implant insertion or pre-implant site preparation were examined. It was found that the majority prescribed AMC 1 g most frequently only after surgical treatment. The tendency to use systemic antibiotics in cases related to the sub-headings of implant surgery was evaluated, it was observed that the most preferred situation was open sinus lift operation with 45%, followed by multiple implant applications and allogeneic/xenogenic bone graft applications with a rate of 41%. It was determined that the same group mostly prescribed AMC (81.9%).
Use of systemic antibiotics in periodontal regeneration & mucogingival surgeries
The participants indicated that they prescribed to their patients systemic antibiotics after guided bone regeneration (83.3%), enamel matrix protein + guided tissue regeneration procedure (62%), guided tissue regeneration (59.3%), and after application of enamel matrix protein (34.3%); 80%, 57.4% and 42.6% of the participants reported that they prescribed systemic antibiotics after allogeneic graft applications (acellular dermal matrix etc.), heterogeneous tissue graft applications (enamel matrix protein etc.) and autogenous tissue graft applications, respectively.
Complications and concerns
Complications and percentages faced by the individuals after prescribing systemic antibiotics were reported as follows: diarrhea 85.2%, abdominal pain 55.6%, nausea-vomiting 50%, urticaria 21.3%, taste disturbance 15.7%, headache 10.2%, and candida infections 5.6%. The greatest concern experienced by those prescribing systemic antibiotics was antimicrobial resistance at 50% and anaphylaxis at 45.4% (Supplementary file). It was determined that the occupational experience and gender of the individuals participating in the study did not show a statistically significant correlation on their preference for prescribing antibiotics in non-surgical periodontal treatment, surgical periodontal treatment and implant surgery (p>0.05).
DISCUSSION
Antibiotics have been used in periodontology for a long time, but information on the prescribing process is limited1,20,21. Following the removal of the appropriate biofilm with the addition of antimicrobial prescription, the level of periodontal disease is assessed, with the invasion of bacteria into tissues being important. The systemic unwellness of the patient with high fever and/or lymphadenopathy, as well as the level of progression of periodontal disease, should be examined in this regard22.
In this study, more than half of the participants stated that they would prescribe single or combined antibiotics in addition to non-surgical periodontal treatment. The antibiotic preferences were in accordance with the recent EFP guideline1. Another reason for this may be that periodontists encounter more advanced forms of periodontitis more frequently than other specialists or dentists. Another explanation may be the different results revealed in randomized controlled clinical studies. While some studies have shown that the use of antibiotics in addition to non-surgical periodontal treatment accelerates wound healing and avoids inflammation and infection16, bacterial resistance development due to antibiotic use has been reported in other studies10.
The results of our study revealed that periodontists prescribe antibiotics more frequently when guided bone regeneration and implant surgery are performed. When infection after periodontal surgeries is evaluated, it has been found that it varies between 0% and 5.88%, with and without antibiotics, respectively, which does not effectively prevent infections6. Despite the information presented, periodontists still frequently use antibiotics after periodontal surgery. This may be related to the belief of dentists that the use of antibiotics will reduce the graft or implant failure rate and that healing will accelerate11. On the other hand, some dentists see grafts and implants as foreign material to the body and that with the use of antibiotics, the primary response to these foreign materials will decrease and thus, less pain will be encountered23.
The other criterion evaluated in our study is the timing of antibiotic use. It was determined that the participants tended to use antibiotics more frequently after surgical/non-surgical periodontal treatment. This result is consistent with the study of Herrera et al.24 on antimicrobial prescription timings. However, in a recent study by Rajendran et al.25 reported that starting antibiotic treatment 6 days before periodontal treatment stimulates post-treatment recovery by reducing IL-1B and Th17. We noted that prescribing AMC was the most common choice in all periodontal treatments. This situation seems to be related to the practice of periodontists to protect their patients from possible secondary infections. Although this result was in accordance with Sanz et al.1 consensus report, a study by Winkel et al.26 revealed that AMC did not have additional protection against periodonto-pathogens.
According to the data we obtained, the participant group stated that they were worried about antimicrobial resistance and anaphylaxis while prescribing systemic antibiotics. A similar result was revealed in the survey study conducted by Ong et al.27 with Australian periodontists. In our study, diarrhea, abdominal pain, vomiting and urticaria were the most common drug complications encountered by dentists.
Limitations
The lack of internal and external validity, the relatively small number of participants and that almost half of the participants had 0–5 years of professional experience, may be considered limitations of this study. Since only 108 individuals participated in the study, the antibiotic prescribing preferences of the periodontist community in Turkey could not be determined precisely. Another possible reason why the participation in the study was less than expected is that the individuals who did not participate may have been more likely to have a negative opinion about the confidentiality of online surveys or needed more spare time for this survey. Despite these limitations, the current study provides valuable information about periodontists’ use of systemic antibiotics in Turkey.
CONCLUSIONS
Our study revealed the tendency of periodontists to prescribe antibiotics in different periodontal conditions, and to the best of our knowledge, this study is one of the few studies conducted in Turkey. The current study has shown the importance of adhering to current guidelines when using systemic antibiotics in periodontal disease, periodontal surgery, and periimplantitis cases. It should be noted that more effective results can be obtained by conducting a large multi-center and multi-participant survey evaluating the antibiotic prescribing trends in different countries.