INTRODUCTION
Nowadays there is a change in lifestyle which translates into a shift in the age of childbearing. Delayed childbearing results in fewer children being born1 while, at the same time, advanced age affects fertility2. Hyperprolactinemia, ovulation disorders, thyroid dysfunction, polycystic ovaries, endometriosis, fallopian tube and uterine abnormalities, infections, autoimmune diseases, neoplasms are causes of infertility3-7. Furthermore, alcohol consumption, caffeine, smoking, obesity, and profession, are among the factors that should be taken into consideration8-10. In the Western world, infertility results in the increasing use of assisted reproduction methods and their further rapid development11. So, infertility has become a social problem with a variety of parameters that need further investigation.
One in six couples worldwide experience some form of infertility problem at least once during their reproductive lifetime12. Infertility lasting for at least 12 months is estimated to affect between 8–18% worldwide of women aged 20–39 years13. In European countries, infertility affects 14% of the population, which means that about one in seven couples is experiencing difficulties.
In Greece, the assisted reproduction field is rapidly evolving and is characterized by parameters that have not been estimated for the majority of the population14. Male infertility was studied during 1992–2008, showing that the male fertility level is declining, the fertility pattern is moving into higher ages, and the reproduction period for men is getting shorter15. Another study focused on fertility variations in the recession context showing that fertility rates in Greece have declined since 201016. No data on infertility of the whole population have been collected up to date and there are no statistical epidemiological data on age, cause of infertility, number of attempts until pregnancy, or even the general profile/background of infertile couples in Greece. The information that can be derived from the largest National Organization for HealthCare Services Provision EOPYY’s data concern almost all Greek insured persons. The present study focused on the general background of infertile people in Greece, as it is the first Social Security registry of infertile people of the country.
METHODS
Study design and participants
Epidemiological data for 9648 patients who applied for assisted reproduction techniques to eight IVF Committees of EOPYY during 2013–2015 were collected. Available data were: committee city, social security ID number, approval date, age of spouses, diagnosis, place of residence, reason for rejection, and center where the attempt would take place. For each approved attempt per unique patient (as determined by its social security ID number) all electronic prescriptions that included medicinal products necessary for the attempt were retrieved by the Department of Prescription Monitoring of EOPYY which has prescription data of the country. Data of these prescriptions were linked to the data of the approvals that EOPYY granted in order to outline the profile of the infertile people covered. This was a secondary dataset analysis since data were obtained from the Committees and Department of Prescription Monitoring of EOPYY.
Further data concerning the outcome of the attempts are under the responsibility of the Greek National Authority of Medically Assisted Reproduction (NAMAR), and EOPYY has no access due to restrictions set by local legislation. NAMAR is responsible for all scientific issues concerning assisted reproduction (licensing, collecting outcome data, reporting) and gave its first report in 2018 which concerned the data of 2014 and 2015. Therefore, the social security data of this study are the first (and latest so far) that are available at national level and can be cross-checked with the respective National Authority’s data. EOPYY’s CEO gave the license for taking and collecting the respective data on 12 March 2013.
Variables
Continuous variables (age, number of cases, number of attempts) are presented as mean and standard deviation, median and range, while nominal variables (residence, method, diagnosis, assisted reproduction center) are presented as frequencies (n) and percentages (%).
Statistical analysis
Relationships between variables were assessed with chisquared test and analysis of variance. Bonferroni post hoc analysis was applied in case of variance analysis. P-values <0.05 were considered as statistically significant. Statistical analysis was performed with the Statistical Package for Social Sciences software (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.).
RESULTS
The sample of the study consisted of 11470 patients. During 2013, 3088 patients applied for an assisted reproduction method approval. During 2014 and 2015 the patients were 3710 and 4672, respectively.
Sociodemographic characteristics and diagnoses of participants
The mean age of women was 36.6 years (SD: 4.8) and the median was 37 years (range: 20–50). The mean age of men was 39.5 years (SD: 5.7) and the median was 39 years (range: 16–74). Women living in five large Greek cities represented 64.7% of those applied for approval.
Regarding the number of attempts, 47.1% (n=3527) of women made two attempts, 41.5% (n=3105) made one attempt, 9.1% (681) made four attempts, and 2.3% (n=173) made three attempts.
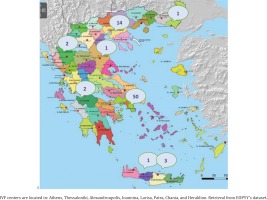
In all, 41.7% of women residing permanently outside Attica/Thessaloniki and 8.9% of women living in Thessaloniki went to an Attica IVF center with this relationship being statistically significant (χ2=6484, p<0.001) (Table 1). In Attica were based 50 of 74 IVF centers (Figure 1).
Table 1
Distribution of the prefecture of the IVF center in relation to the prefecture of residence, 2013–2015 (N=11470)
The most common method was IVF (86.1%) followed by ovulation induction (10.5%), sperm injection (2%) and administration of hormones (gonadotropins) to men (1.3%).
It was found that 45.7% of cases (i.e. 5249 cases) were related to female reproductive system problems, 41% of cases (4713 cases) were related to male factors, while 13% (1509 cases) were related to problems encountered by both prospective parents.
The most common diagnoses (Table 2) were abnormal semen parameters, male factor and increased sperm adhesion (39.9%). In a total of 11470 cases, 1275 had two diagnoses (11.1% of the cases). The most common second diagnoses were failed sperm inseminations and ovulation inductions (n=481) and abnormal sperm parameters, male factor, increased sperm adhesion (n=396).
Table 2
Most common diagnoses, 2013–2015 (N =11470)
Association between sociodemographic characteristics and diagnoses/assisted reproduction method
Statistically significant relationships were found between age and other diagnoses (p<0.001) as shown in Table 3. In azoospermia, mean age was lower than abnormal semen parameters, male factor, increased sperm adhesion, anovulation, low AMH, infertility, failed sperm inseminations and ovulation inductions, fallopian tube obstruction, tubal factor, and tubal symphysis (p<0.001). In abnormal semen parameters, male factor and increased sperm adhesion, the mean age was lower than anovulation, low AMH, infertility, failed sperm inseminations and ovulation inductions, fallopian tube obstruction, tubal factor, and tubal symphysis (p<0.001). In pre-implantation diagnosis, mean age was lower than anovulation, low AMH, infertility, failed sperm inseminations and ovulation inductions, fallopian tube obstruction, tubal factor, and tubal symphysis (p<0.001). In anovulation and low AMH, the mean age was higher than hypogonadotropic hypogonadism and PCOS. In sperm inseminations and ovulation inductions, the mean age was higher than hypogonadotropic hypogonadism, fallopian tube obstruction, tubal factor, tubal symphysis, salpingectomy, and PCOS and endometriosis. In PCOS, the mean age was lower than in all other cases (p<0.001).
Table 3
Distribution of diagnosis according to age, 2013–2015 (N=11470)
IVF was statistically significantly more common in all diagnoses except in the case of hypogonadotropic hypogonadism where hormone administration was more commonly used in men (p<0.001) (Table 4). Apart from diagnoses where IVF was one way solution (i.e. cancer or pre-implantation genetic diagnosis), it seems that it was also the prevalent method in cases of abnormal semen parameters (93.9 %) and infertility which could not be attributed to other causes (79.0%).
Table 4
Distribution of methods applied according to the diagnosis, 2013–2015 (N=11470)
Women who performed IVF had a statistically significantly higher mean age than those using the other methods (p<0.001) since the mean age for IVF was 36.9 years, whereas the mean age for ovulation induction was 35.1 years and for sperm insemination it was 34.7 years.
Most women of those that did an assisted reproduction method were aged 25–35 years while there was a clear preference for IVF in women over 35 years (Table 5).
Table 5
Number of patients per method and age group, 2013–2015 (N=11470)
| Method | Age (years) | Number of patients |
|---|---|---|
| IVF | * | 353 |
| <25 | 43 | |
| >45 | 263 | |
| 25–35 | 3635 | |
| 36–37 | 1448 | |
| 38–40 | 2103 | |
| 41–45 | 2034 | |
| Ovulation induction | * | 42 |
| <25 | 11 | |
| >45 | 1 | |
| 25–35 | 619 | |
| 36–37 | 192 | |
| 38–40 | 221 | |
| 41–45 | 123 | |
| Sperm injection | <25 | 5 |
| >45 | 3 | |
| 25–35 | 133 | |
| 36–37 | 36 | |
| 38–40 | 34 | |
| 41–45 | 20 | |
| Hormone administration to men | * | 88 |
| <25 | 4 | |
| 25–35 | 32 | |
| 36–37 | 14 | |
| 38–40 | 12 | |
| 41–45 | 1 |
DISCUSSION
In European countries infertility affects 14% of the population13. In 2016, Spain was the most active IVF country in Europe followed by Russia, France, Germany, Italy, and UK12. In Greece, no data on infertility have been collected up to date on behalf of Social Security Institutions. Data of this study relate to the part of the population that decided to use an assisted reproduction method covered by its Social Insurance. It is understood that infertility affects a larger proportion of the population and in many cases it has not yet been diagnosed, and many couples do not wish to use assisted reproduction methods or they prefer to cover all the costs on their own. Data collection and monitoring is performed both by EOPYY and NAMAR. EOPYY has realworld data while NAMAR has a time lag of about 3 years (first report of NAMAR so far was on 2018 regarding data of 2014 and 2015). According to legal framework, only NAMAR is informed by the assisted reproduction units of the outcome of the efforts.
EOPYY has strict guidelines and a maximum of 4 efforts per woman is approved and reimbursed. In the period 2013–2015, EOPYY granted approvals for the performance of 10889 cycles. A total of 3285 approvals were for one cycle, while 3802 approvals were for two cycles. This means that in Greece there is an average of 3629 IVF cycles each year covered by EOPYY. According to NAMAR, 28361 cycles were recorded on 2014 and 30728 cycles for 2015, resulting in 5854 and 7036 newborns, respectively17, showing that many efforts are carried out privately.
According to this study, the mean age of women was 36.6 years, while that of men was 39.5 years. The majority of women were aged 35–39 years (37%, 4173), while the proportion of women over 40 was 29% (3207). According to the European Society of Human Reproduction and Embryology (ESHRE) 2016 ART fact sheet, most treatments were performed on women aged 30–39 years, whereas 2017 fertility success rates data of CDC show that over 80% of women that have undergone ART procedures were up to 40 years of age12. Only 2% of women examined by assisted reproductive committees were over 45 years old (267 persons) given the low probability of these methods being successful in this age group. This is in line with the literature as the observed decrease in fertility is greater between 40 and 44 years, and after 45 years only a fraction of 2–5% of women are able to have successful pregnancies18.
The method of choice was in vitro fertilization at 86.1%. It should be noted that this figure includes Intra-cytoplasmic Sperm Injection (ICSI) cases as it was not feasible to separate these cases in data we received from EOPYY. These data are consistent with the statistics data on medically assisted reproduction units presented by the NAMAR at the ESHRE conference in Barcelona in 201817. According to the Authority, in the year 2015, 14% proceeded with sperm insemination, while the rest (86%) used in vitro fertilization (IVF or ICSI). Given the normal decline in fertility over age, it is logical for health professionals to focus more on active methods of assisted reproduction to deal with fertility problems. Women who performed IVF had a statistically significantly higher mean age (36.9 years) than those using other methods. A new study that took place in Southern Brazil also showed that most cases of assisted reproductive technology were by in vitro fertilization (70.6%) and ART-mothers were in general older than mothers who had spontaneous pregnancies19.
In 50% of cases, infertility is attributed to female reproductive system problems, while 30% is attributed to male factors. Finally, in 20% of cases, infertility is thought to be due to problems of both sexes20. According to other research, there is a male factor in 25–40% of infertile couples, whereas the ovarian factor is responsible for female infertility in 30–40% of cases21. According to this study, problems are found to a similar degree in both sexes (45.7% female and 41% male reproductive system problems). Unexplained infertility was reported in 11% of the cases studied (1208 cases), consistent with what ESHRE reports, i.e. in 10–20% of cases there is no apparent cause of infertility12. Additionally, this finding is in agreement with 2017 fertility success rates data of CDC which reported 11% for unexplained infertility22.
In the present study, the necessity of using IVF is also indicated by the most common diagnoses which are abnormal sperm parameters, male factor, increased sperm adhesion, fallopian tube obstruction, tubal factor, tubal symphysis, anovulation and low AMH, infertility, and azoospermia. Infertility includes diagnosis of primary and secondary fertility, miscarriages, failed IVF, and early menopause. In addition, IVF appears to be the only choice as, among the 11470 cases, in 1275 (11.1%) there were more diagnoses, the most common of which were failed sperm insemination and ovulation inductions (n=481); abnormal sperm parameters, male factor, increased sperm adhesion (n=396), fallopian tube obstruction, tubal factor, tubal symphysis (n=195), i.e. problems that can only be resolved with in vitro fertilization. Regarding the contribution of male factor, these findings were slightly different from those presented by ESHRE 2016 ART fact sheet according to which 20–30% of infertility cases are explained by physiological causes in men12. Furthermore, 2017 fertility success rates data of CDC reported that the reason for an attempt was the male factor in the 28% of cases22. According to our data, the contribution of male factor seemed to be even higher in cases where there was a relative second diagnosis.
The 88.6% of women with infertility problems are doing one or two assisted reproductive efforts at most (in vitro fertilization, ovulation induction, sperm insemination), avoiding being approved for two additional attempts by EOPYY. In cases of ovulation induction and sperm insemination, this is a signal for their turn to IVF, whereas in cases of IVF this is a signal for demonstrating skepticism of patients and their physicians against two additional efforts that require additional thousands of units of gonadotropins as medication. These data correspond to data mentioned in a relevant guideline given by the National Health System of the United Kingdom. According to a study conducted on the number of previous failed IVF cycles during the period 1991–1994, the probability of success decreases in each cycle from 14% in the first attempt to 13% in the second, 11.4% in the third23 and 9.3% in the fourth attempt. Additionally, data collected by the Human Fertilization and Embryology Authority (HFEA) showed that the percentage of IVF cycles that resulted in births decreases from 20% when the mother is aged 38–39 years, to 12.3% at age 40–42 years, and to just 4.9% when she is over 42 years24.
During the study period, there were 158 cases of women who stated that they would use donor semen. Of these, 149 requested approval for IVF, 8 to induce ovulation, and one for sperm insemination. In addition, there were 4 cases of surrogate mothers and no cases of female HIV carriers wishing to conceive using assisted reproduction methods. Τhis fact characterizes Greek society’s view of the family and the triptych ‘father-mother-child’. Women in today’s Greece will find it difficult to turn to the sperm donor or surrogate mother as they want to exhaust all available (medical and non-medical) childbirth opportunities in a way that meets the standards set by the society in which they live25,26.
The majority of women who came to EOPYY IVF Committees were living in large urban centers. This finding agrees with previous research showing that the majority of women dealing with infertility live in cities27,28. Maybe the higher educational level combined with better career possibilities in cities could drive women to postpone motherhood27,29. Furthermore, general lifestyle conditions in cities (smoking, alcohol, caffeine, occupation or lack of exercise) may contribute to the observed fertility decline.
Limitations
The main limitation of this study was that it was not possible to know the outcome of each effort funded by EOPYY, since these data are reported only to NAMAR by IVF units. Furthermore, it was not possible for EOPYY to detect which IVF cases are referring to the classic IVF method and which to an ICSI method performed. Finally, it was not feasible to collect data for those women who used IVF services at their own expense.
CONCLUSIONS
During 2013–2015, there was an annual average of 3629 IVF cycles performed in the country (mainly in the capital, Athens) and reimbursed by EOPYY. Infertility was mainly attributed to abnormal sperm parameters, increased sperm adhesion, fallopian tube obstruction, tubal factor, and tubal symphysis. Problems of the female reproductive system are found in a similar percentage to problems of male etiology. Greece follows the European pattern since most patients were aged 30–39 years, did mostly In Vitro Fertilization/ICSI and received approval for one to two attempts at most, mainly with their own sperm. Inexplicable infertility was reflected in 11% of cases in this study, whereas a very small percentage of women over 45 years had undergone some method.
Women and men should be informed at a young age about factors affecting fertility. Specialized training programs could be developed for this purpose. Specific and targeted actions should be designed to ensure full information and awareness of young ages in order to prevent situations that can lead to fertility disorders. Since EOPYY’s guidelines set a strict administration framework, many efforts were made at the expenses of the patients. EOPYY-NAMAR cooperation is considered absolutely necessary in order the risk/benefit ratio to be assessed. Sharing data regarding outcomes will give Social Insurance the ability to re-evaluate reimbursement procedures and lead to evidence-based legislation updates.