INTRODUCTION
Cardiovascular disease (CVD) is the leading cause of mortality in the United States, accounting for a third of deaths1. Despite numerous prevention and cessation efforts, tobacco smoking persists as a significant, though preventable, risk factor for heart disease2 as well as a key contributor to overall mortality3. Although death from CVD typically occurs later in life, recent estimates project that 5.6 million current teens will experience premature death from smoking-related diseases3. Most smokers in the US begin smoking before the age of 18 years, predisposing them to lifetime addiction3. Despite many programs designed to raise awareness and dissuade youth from using tobacco products, tobacco use is prevalent among US high school and middle school students. In 2020, for example, 23.6% of high school and 6.7% of middle school students reported current use of any tobacco product4.
Youth may trivialize the risks associated with smoking and overrate their ability to quit tobacco use5, which may influence them to initiate and continue using tobacco products. For example, youth with a history of smoking are more likely to report lower risk perceptions of cigarette use6. Some youth view themselves as immune to tobacco-related disease7, and lower perceptions of long-term smoking risks may increase the likelihood of smoking8. Additionally, despite public health efforts9, many youth have positive perceptions of smoking. These positive perceptions include fostering a sense of belonging in peer groups, indicating one’s ‘coolness’, providing an outlet for stress, and offering enjoyment10.
Research examining CVD risk perceptions related to tobacco use among youth is limited. This gap in the literature warrants an examination of how CVD risk perceptions relate to tobacco use behaviors. Some research has found that youth and young adults perceive that their risk for developing CVD is low11. Certainly, recommendations to reduce CVD risk highlight preventing tobacco use and quitting12. Therefore, examining drivers of associations between tobacco use and CVD risk perceptions among youth may help clarify factors that facilitate or hinder tobacco prevention initiatives, especially among underrepresented populations.
Tobacco product use is higher among American Indians/Alaska Natives, LGBTQ populations, individuals with lower income, and rural populations13,14. A clear relationship exists between lower household income and higher smoking prevalence15. For example, individuals living below the poverty line are more likely to smoke16, are less successful at quitting3, and live in neighborhoods with more tobacco retailers17. Also, compared to urban dwellers, rural residents are more likely to report current smoking14.
This study focused on youth living in Appalachia, a region where socioeconomic disadvantages18 and high tobacco use rates are prevalent19. For example, nearly one-fifth (19.8%) of the population in Appalachia smokes, which exceeds the US national average (16.3%) as well as estimates for regions outside Appalachia (16.0%)19. To date, literature examining tobacco use and risk perceptions among Appalachian youth is sparse. One study reported that Appalachian youth who used combustible cigarettes, compared to youth who had never used tobacco products, had higher odds of disagreeing that smoking causes health problems and addiction20. As CVD remains a leading cause of death, it is important to investigate whether CVD risk perceptions among Appalachian youth are associated with tobacco use. Therefore, this study aims to: 1) examine the association of tobacco use status and CVD risk perceptions, and 2) investigate the sociodemographic correlates of associations between tobacco use status and CVD risk perceptions.
METHODS
Data collection
Data used in this study were obtained from the Youth Appalachian Tobacco Study (YATS), which surveyed middle and high school students in the Appalachian regions of Kentucky, North Carolina, and New York between fall 2014 and spring 2016. Informed consent was obtained before data collection. Parents were provided a letter describing the study and could elect to allow or decline their child’s participation. Assent forms were given to students, and they could decline participation as well. The investigator-generated questionnaire included items on sociodemographic characteristics, tobacco use perceptions, tobacco use behavior, and tobacco marketing and advertising. Ethical approval was obtained from the Institutional Review Board of the University of Louisville.
Participants
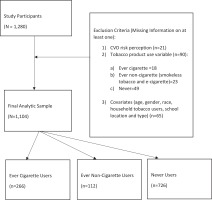
A total of 1280 middle and high school students participated in YATS. Participants were excluded from this analysis if they did not respond to questions on CVD risk (n=21), had missing information on tobacco product use (n=90), or had missing information on sociodemographic characteristics (n=65) (Figure 1). The final sample included 1104 participants.
Primary measures
Tobacco use status was defined by ever cigarette, e-cigarette, and smokeless tobacco use. Participants who reported having ever used cigarettes were classified as ever cigarette users. Participants who reported having never used cigarettes but who had used e-cigarettes or smokeless tobacco products were classified as ever non-cigarette users. Participants who reported having never used any tobacco product were classified as never users. These user groups were selected as perceptions of CVD risk likely vary by youth who use cigarettes and youth who use other tobacco products, such as e-cigarettes or smokeless tobacco.
CVD risk perceptions were determined by participants’ agreement or disagreement with the following statements: ‘Smoking causes heart disease’, ‘Smoking causes strokes’ and ‘Smoking causes high blood pressure’. A 5-point Likert scale was employed with response options indicating level of agreement with each statement (1=Strongly Disagree, 2=Disagree, 3=Neither Agree/Disagree, 4=Agree, 5=Strongly Agree). Responses were dichotomized (i.e. responses 1–3=Disagree, responses 4–5=Agree). Each CVD risk perception (i.e. heart disease, stroke, high blood pressure) was examined separately.
Sociodemographic characteristics such as gender (male, female), race/ethnicity, school type (middle school, high school), state (Kentucky, New York, North Carolina), and household tobacco use (no household users, one or more household users) were analyzed. Participants identified as either White, Black/African American, Hispanic, Asian, Other, or two or more races. Race/ethnicity was dichotomized into White and racial/ethnic minorities.
Statistical analysis
Sociodemographic characteristics by CVD risk perceptions and tobacco use status were evaluated using chi-squared test of independence for categorical variables and analysis of variance (ANOVA) for continuous variables. Further, pairwise tests were conducted to compare among tobacco use groups (i.e. ever cigarette users, ever non-cigarette users, and never users) by descriptive characteristics and CVD risk perceptions using chi-squared test of independence, Fisher’s exact test or Student’s t-test, where appropriate.
Three logistic regression models, one per CVD risk perception statement (i.e. smoking causes heart disease, smoking causes strokes, and smoking causes high blood pressure), were performed to examine associations between tobacco use status and CVD risk perceptions after adjustment for household tobacco use, race/ethnicity, and gender. The exposure reference group was never users, and the outcome reference group was agreeing with CVD risk statements. Adjusted odds ratios (AORs) and 95% confidence intervals are reported. Results were considered statistically significant at α=0.05. Data were analyzed using SAS statistical software, version 9.421.
RESULTS
Sociodemographic characteristics by tobacco use status
The sample included 1104 youths with ages ranging from 11–19 years (mean±SE: 13.8±0.1). The majority were male (n=560; 50.7%), White (n=980; 88.8%), in middle school (n=665; 60.2%), living in North Carolina (n=512; 46.4%) or Kentucky (n=377; 34.1%), and living with at least one tobacco user (n=633; 57.3%) (Table 1). Of the sample, 65.8% were never users, 24.1% ever cigarette users, and 10.1% ever non-cigarette users. Significant differences were found between tobacco use status and sociodemographic characteristics (Table 1), except for race/ethnicity (p=0.419). More ever cigarette users were male (51.5%), in high school (57.9%), in Kentucky (47.4%), and living with a household tobacco user (75.2%), compared to never users (48.8%, 31.5%, 28.4% and 50.4%, respectively). More ever non-cigarette users were male (62.5%), White (91.1%), from Kentucky (40.2%) and living with a household tobacco user (59.8%), compared to never users (48.8%, 87.9%, 28.4% and 50.4%, respectively). Of ever cigarette users, nearly one-fifth (19.2%) disagreed that smoking causes heart disease (p=0.001) and approximately one-fourth (24.8%) disagreed that smoking causes strokes (p=0.006), compared to 10.3% and 16.3% of never users, respectively. Additionally, 15.2% of ever non-cigarette users disagreed that smoking causing high blood pressure, compared to 18.7% of never users (p=0.024).
Table 1
Participant characteristics by tobacco use status, Youth Appalachian Tobacco Study, USA, 2014–2016 (N=1104)
Sociodemographic characteristics by CVD risk perceptions
Sociodemographic characteristics by CVD risk perceptions (smoking causes heart disease, smoking causes strokes, and smoking causes high blood pressure) are shown in Table 2. Approximately 12.9% of the sample disagreed that smoking causes heart disease (Table 2). More males than females (59.2% vs 40.8%, p=0.033), middle schoolers than high schoolers (68.3% vs 31.7%, p=0.035), and youth residing in Kentucky (46.5%) and North Carolina (41.5%) than in New York (12.0%) (p=0.002) disagreed that smoking causes heart disease. No differences were found by race/ethnicity.
Table 2
Participant characteristics by cardiovascular disease risk perceptions, Youth Appalachian Tobacco Study, USA, 2014–2016 (N=1104)
With regard to stroke, 18.9% of the sample disagreed that smoking causes strokes (Table 2). More youth with a household tobacco user than those without one (67.0% vs 33.0%, p=0.002) disagreed that smoking causes strokes (Table 2). Statistically significant differences were not observed by gender, race/ethnicity, school type, or state.
Approximately 20% of the sample disagreed that smoking causes high blood pressure (Table 2). More middle schoolers than high schoolers (68.8% vs 31.2%, p=0.004) disagreed that smoking causes high blood pressure. Also, differences were observed by race/ethnicity (p<0.001) but not gender or state.
Logistic regression results
After adjustment for gender, race/ethnicity, and household tobacco use, ever cigarette users had 83% higher odds of disagreeing that smoking causes heart disease, compared to never users (AOR=1.83; 95% CI: 1.23–2.73) (Table 3). Ever non-cigarette users had 33% higher odds of disagreeing that smoking causes heart disease compared to never users (AOR=1.33; 95% CI: 0.74–2.39), although this result was not statistically significant. Also, after adjustment for tobacco use status, youth with a household tobacco user had 71% higher odds of disagreeing that smoking causes heart disease when compared to those without one (AOR=1.71; 95% CI: 1.15–2.54). Additionally, compared to males, females had 31% fewer odds of disagreeing that smoking causes heart disease (AOR=0.69; 95% CI: 0.48–0.99).
Table 3
Multivariable logistic regression models estimating associations between tobacco use status and each CVD risk perception, Youth Appalachian Tobacco Study, USA, 2014–2016 (N=1104)
With regard to stroke, ever cigarette users had 54% higher odds of disagreeing that smoking causes strokes compared to never users (AOR=1.54; 95% CI: 1.08–2.18). Ever non-cigarette users had 41% higher odds of disagreeing that smoking causes strokes compared to never users (AOR=1.41; 95% CI: 0.86–2.31), though the difference was not statistically significant. Youth who identified as White had 35% fewer odds of disagreeing that smoking causes strokes compared to racial/ethnic minorities (AOR=0.65; 95% CI: 0.41–1.04). Also, youth with a household tobacco user had 59% higher odds of disagreeing that smoking causes strokes compared to those without one (AOR=1.59; 95% CI: 1.15–2.22).
Ever cigarette users had 41% higher odds of disagreeing that smoking causes high blood pressure when compared to never users (AOR=1.41; 95% CI: 1.00–1.99). Ever noncigarette users had 25% fewer odds of disagreeing that smoking causes high blood pressure when compared to never users (AOR=0.75; 95% CI: 0.43–1.31), although this result was not statistically significant. Also, youth who identified as White had 56% fewer odds of disagreeing that smoking causes high blood pressure compared to racial/ethnic minorities (AOR=0.44; 95% CI: 0.29–0.68).
DISCUSSION
To our knowledge, this study is among the first to assess the relationship between tobacco use status and CVD risk perceptions among Appalachian youth. Results showed that youth perceptions of smoking and its association with CVD risks varied by tobacco product use, with ever cigarette users having higher odds of disagreeing that smoking causes heart disease, stroke, and hypertension, compared to never users. These findings are concerning, as lower perceptions of smoking-related risks, such as the incidence of heart disease, stroke, and hypertension, may contribute to continued tobacco use among youth22. Our findings, however, lend support to previous research indicating that cigarette users have lower perceptions of smoking-related risks23,24. Additional anti-tobacco messages aimed at effectively communicating the dangers of smoking, including CVD risks, are needed, especially among Appalachian youth.
It is important to understand the association between tobacco use behaviors and CVD risk perceptions among youth, as this group is intentionally targeted by tobacco companies with the aim of lifetime purchasing and use25,26. However, despite this knowledge and the evidence of greater tobacco use by low-income rural youth, there is inadequate enforcement of regulations designed to protect youth living in low socioeconomic rural areas26. Development and implementation of culturally sensitive anti-tobacco programs for disproportionately affected groups, such as Appalachian youth, is critical for addressing health inequities. Future research should aim to examine the mechanisms behind higher prevalence of tobacco use among Appalachian populations, and its association with lower risk perceptions of smoking-induced heart disease, stroke, and hypertension.
Although not statistically significant in the adjusted multivariable logistic regression, ever non-cigarette users (e-cigarette and smokeless tobacco users) had fewer odds of disagreeing that smoking causes hypertension compared to never users, which differs from previous research findings of lower risk perceptions among youth who use electronic cigarettes, smokeless tobacco products, or more than one tobacco product20,24. The non-significant finding after adjustment in the regression analysis is possibly due to the low prevalence of ever non-cigarette users in our sample. It is also possible that these youth use electronic cigarettes and/or smokeless tobacco rather than cigarettes because they are more aware of the risks of cigarettes or perhaps, due to messaging (e.g. social media), they perceive these products as safer alternatives to cigarettes27.
Youth perceptions of smoking causing heart disease, stroke, and hypertension, varied by sociodemographic characteristics, with youth who had at least one household tobacco user having higher odds of disagreeing that smoking causes heart disease, stroke, and hypertension. This outcome supports previous findings of lower perceptions of smokingrelated harm in youth who have a household member that uses tobacco28-30. It is conceivable that youth who are exposed to a home environment where tobacco is used are more likely to view tobacco use behavior as normal and thus less harmful than youth who are not. Health messaging and strategies focused on the denormalization of tobacco use behavior among youth in Appalachia are needed. Strategies aimed at curbing tobacco use among adults may subsequently affect youth, reducing use in both populations. Youth who identified as racial/ethnic minorities had higher odds of disagreeing that smoking causes hypertension, which is a significant cause for concern, as racial/ethnic minorities, such as African Americans, Hispanics/Latinos, and Asians, tend to have higher rates of hypertension compared to Whites31,32. For Appalachian youth smokers who do not perceive smoking to cause CVD, tobacco prevention and cessation efforts are especially important because previous studies have found associations between tobacco exposure and elevated blood pressure among youth, including racial/ethnic minority youth and rural youth33,34. Tobacco messaging may not be reaching racial/ethnic minorities; therefore, carefully targeted campaign messages aimed at racial/ethnic minority youth in the Appalachian region are crucial. Also, public awareness campaigns should aim to eliminate misunderstanding about smoking-related risks among racial/ethnic minority youth in the Appalachian region.
We also found that females had fewer odds of disagreeing that smoking causes heart disease compared to males, which corroborates previous research indicating that females are more likely to view smoking as harmful29. We postulate that males have lower perceptions of smoking-related heart disease risks, as males tend to have more self-exempting beliefs regarding tobacco-related disease35. Our work calls for future research to further examine the associations of gender and race/ethnicity among Appalachian youth tobacco users to better understand the intersectionality of CVD risk perceptions and tobacco product use.
Limitations
There are several limitations to this study. First, we relied on self-reported responses, which are subject to potential biases, such as recall and social desirability. Second, the data are from three states and may not represent all youth in living in the Appalachian region. Another limitation is that we aggregated race and ethnicity data. Finally, this study was done prior to the COVID-19 pandemic and does not reflect potential changes that may have occurred due to the pandemic. However, despite the limitations, findings from this study are important for future research and tobacco prevention efforts, especially work involving Appalachian youth.
CONCLUSIONS
We examined associations between tobacco use status and perceptions of CVD risk among Appalachian youth. Tobacco use status and household tobacco use were associated with disagreement that smoking causes heart disease, hypertension, and stroke. Appalachian youth CVD risk perceptions also varied by gender and race/ethnicity. The findings of our study emphasize the need for further health education efforts aimed at improving youth understanding of tobacco use risks in the Appalachian region. Further, males and racial/ethnic minorities are disproportionately affected by tobacco use, and additional health communication campaigns are needed to promote health equity among Appalachian youth.