INTRODUCTION
Diabetes is a major health concern worldwide, and Africa is disproportionately impacted by rising prevalence and the highest rate of undiagnosed people with diabetes1-3. Diabetes is heterogeneous, consisting of not just the common/prevalent type 1 and type 2 diabetes but less common types, including monogenic diabetes, of which Maturity-Onset Diabetes of the Young (MODY) is the commonest form4. Data from Western nations show that the prevalence of MODY is between 2–4% of the diabetes population5, and approximately 90% of cases are undiagnosed6. However, accurate diagnosis and classification are imperative to precision diabetes medicine because it drives treatment selection to optimize glycemic control.
MODY is a single-gene heterozygous group of disorders characterized by autosomal dominant inheritance7. To date, at least fourteen different genes have been implicated as causing MODY (with some under debate). MODY, due to pathologic variants in the hepatocyte nucleocyte factor 1-alpha (HNF1a), Glucokinase (GCK), and hepatocyte nucleocyte factor 4-alpha (HNF4a) genes are the commonest subtypes8. Routine genetic diagnosis of MODY has become feasible due to rapid progress in molecular genomics. Unlike developed countries, awareness and diagnostic uptake of MODY remains very low in Africa, including Nigeria3,9. It is unclear if healthcare professionals (HCPs) in sub-Saharan Africa are aware of and/or apply existing guidelines on the diagnosis and treatment of monogenic diabetes8,10, as there is very little reporting of the condition. It is important to identify and confirm the diagnosis of MODY before effective personalized treatment of the various subtypes can be instituted11-13. Classically, HNF1A-MODY and HNF4A-MODY respond very well to sulfonylureas while GCK-MODY requires no treatment.
Previous studies have identified a lack of knowledge and awareness among HCPs in Western nations as one of the barriers to genetic testing for MODY14,15. Low MODY knowledge and awareness among HCPs may also be contributing to the underdiagnosis of MODY in Africa, including Nigeria, but this has not been investigated. The purpose of this study was to assess knowledge of and clinical experience with MODY among HCPs in Nigeria, as a vital step towards the implementation of precision diabetes medicine in the country and the African continent.
METHODS
Design and instrument
A cross-sectional survey was carried out among physicians and nurse practitioners in the Ibadan metropolis, Nigeria.
Sampling and recruitment
The survey was carried out from December 2018 to June 2019 in all the 11 local government areas within the Ibadan metropolis. Ibadan is the largest city by geographical area in the whole of West Africa and the third largest city in the region by population size. A sample size of 400 HCPs in both public and private hospitals was targeted. Ibadan, like the rest of the country, has three levels of public health institutions: primary, secondary, and tertiary, and several private hospitals scattered in each local government. There were 67 primary health centers (PHCs), five secondary health hospitals, and one tertiary-level care. There were more HCPs in public compared to private hospitals; the only tertiary health institution, the University College Hospital (UCH), has the largest number of HCPs, followed by the secondary hospitals, private hospitals, and PHCs in that order. The proportion of participants set to be sampled in the recruitment sites was divided according to the following ratio: public and private=70:30. Allotted percentages for public health facilities were further subdivided as follows: tertiary=40%, secondary=20%, primary health centers=10%; private=30%. Doctors and nurses were projected to be recruited at a ratio of 60:40, respectively.
The tertiary hospital (UCH) and all five secondary (general) hospitals were visited. At the tertiary and secondary hospitals, participants were recruited from departments/clinics where diabetes patients were seen. These departments were general/family, internal medicine, and clinical chemistry/chemical pathology laboratory. The allocated number of PHC and private hospitals in each local government were randomly selected by simple balloting from a list obtained from the state ministry of health. All consenting HCPs who, at the time of recruitment, had seen or expected to be part of the management team of diabetes patients were eligible and consecutively recruited until the assigned number of participants in each category was reached. A total of 415 out of 432 participants responded, giving a response rate of 96%.
Trained research assistants visited each designated healthcare facility and delivered hard copies of the questionnaire to consenting HCPs in the facility. The facility was visited again within two days to retrieve the completed questionnaires. Participants yet to complete surveys were reminded via mobile telephone calls and then visited again. Any participant who had not completed the survey after three attempts was then excluded from the study.
The survey instrument was developed through an iterative process utilizing expert consultation from genetic epidemiologists at the University of Chicago Survey Laboratory, USA, and was followed by face-to-face validation with experienced clinical experts in monogenic diabetes from the University of Chicago Monogenic Diabetes Registry, to ensure its reliability. The instrument was further fine-tuned to reflect the context of the Nigerian healthcare system. Finally, the pre-testing interview was done in a community that was excluded from the study sites for clarity, consistency of questions, and overall validation of the instrument. Ambiguous questions were modified based on feedback. There were five sections (section A-E) and a total of 51 survey items in the instruments (Supplementary file Tables 1 and 2).
Section A consisted of questions to test the understanding of basic genetic concepts; section B sought the views of HCPs on the role of genetic testing in the diagnosis of diabetes; questions in section C evaluated barriers to genetic testing applicable to diabetes; section D specifically queried on knowledge of diagnosis and treatment of MODY; and section E collected demographic data from respondents. The questionnaire was designed to be self-administered with an estimated completion time between 15 and 20 minutes.
Statistical analysis
Data were summarized using means and standard deviation for quantitative variables and frequencies and proportions for qualitative variables. Aggregate scores were computed for five questions on knowledge of basic genetics (maximum score of 5) and nine items that directly tested for MODY-specific knowledge (maximum score of 9). Age-dependent differences in the knowledge of basic genetics and MODY and adequacy of training exposures to the use of genetic testing were computed. Basic genetics knowledge scores were further compared among categories of sociodemographic and work-related variables using t-tests and analysis of variance. Multiple linear regression was done to determine variables associated with basic genetics knowledge scores, and regression coefficients and their 95% confidence intervals are reported. Statistical significance was set at p<0.05.
RESULTS
Sociodemographic characteristics
There were 415 HCPs comprising 254 (61.2%) doctors and 161 (38.8%) nurses; 156 (37.6%) worked in public tertiary health facilities, 148 (35.7%) in other public tiers of care, while 111 (26.7%) worked in private health facilities. The median age was 39 years (range: 22–71), and 256 (61.7%) were females (Table 1).
Table 1
Demographic characteristics of healthcare practitioners in a survey within the Ibadan metropolis, Nigeria, 2018–2019 (N=415)
Genetics knowledge
A total of 119 (43.4%) respondents self-rated their knowledge of MODY to be at least moderate (Table 1). Of all the participants, 67.5%, 72.6%, and 86.2%, respectively, correctly answered 3 out of 5 questions posed to test basic genetics knowledge (Table 2). In contrast, only 1 out of 7 MODY-specific questions was correctly answered by the majority (72.7%) of the participants. Compared to the older (aged ≥40 years) respondents, higher percentages of the younger ones significantly performed better in 2 of the basic genetics knowledge questions (61.5% vs 38.5%; 57.6% vs 42.4%, respectively), while greater percentage (53.7% vs 46.3%) of the older respondents performed better in one question. There were no significant differences in performance between the two age groups in all the MODYspecific knowledge.
Table 2
Comparison of basic genetics knowledge between younger (aged <40 years) and older (aged ≥40 years) groups among surveyed healthcare professionals in hospitals within the Ibadan metropolis, Nigeria, 2018–2019 (N=415)
| Knowledge domain | All n (%) | Younger (<40 years) n (%) | Older (≥40 years) n (%) | p |
|---|---|---|---|---|
| Basic genetics knowledge score | ||||
| Genetics refers to the interaction of genes with one another (True) | 95 (23.6) | 44 (46.3) | 51 (53.7) | 0.014* |
| A version of a gene in a locus is named an allele (True) | 260 (67.5) | 160 (61.5) | 100 (38.5) | 0.002* |
| Mitochondrial inheritance is not a pattern of Mendelian inheritance (Correct) | 283 (72.6) | 149 (52.7) | 134 (47.3) | 0.121 |
| A diagram of historical genetic relationships in a family using standard symbols is a family tree/pedigree (Correct) | 349 (86.2) | 189 (54.2) | 160 (45.8) | 0.927 |
| Multiplication is not a type of genetic mutation (True) | 132 (34.9) | 76 (57.6) | 56 (42.4) | 0.036* |
| MODY specific knowledge | ||||
| First-line treatment for HNF1A-MODY (Sulfonylureas) | 41 (11.3) | 27 (65.9) | 14 (34.1) | 0.087 |
| First-line treatment for GCK-MODY outside of pregnancy (No treatment) | 9 (2.5) | 5 (55.6) | 4 (44.4) | 0.221 |
| Minimum age respondent would consider a diagnosis of MODY (Newborn) | 28 (7.6) | 17 (60.7) | 11 (39.3) | 0.487 |
| The family history consistent with a MODY diagnosis (including the proband, there are 2, 3, 4 or more generations of diabetes) | 104 (29.2) | 64 (61.5) | 40 (38.5) | 0.149 |
| The autoantibody scenario respondent would consider a diagnosis of MODY (no positive Islet cell autoantibodies) | 59 (16.4) | 34 (57.6) | 25 (42.4) | 0.676 |
| Treatment history that would make respondent consider a diagnosis of MODY (no past or current treatment with insulin) | 69 (19.9) | 42 (60.9) | 27 (39.1) | 0.254 |
| Top three factors considered most important for MODY diagnosis (any 3 out of: age at diagnosis, BMI, family history, Islet autoantibody status, and insulin treatment) | 250 (72.7) | 138 (55.2) | 112 (44.8) | 0.610 |
The mean basic genetics knowledge score was 2.6 (out of 5) (SD=1.0). It was significantly higher among doctors (mean=2.8; SD=1.0) compared to nurses (mean=2.3; SD=1.0) (p<0.001). Also, the mean MODY-specific knowledge score was 1.8 (SD=1.3) from a maximum score of 9 from 9 items. The mean score was higher for doctors (mean=1.9; SD=1.4) compared to nurses (mean=1.7; SD=1.2) (p=0.057). Significant associations were found between basic genetics knowledge scores and age (p=0.025), education level (p=0.002), and cadre (p<0.001) on bivariable analysis (Table 3). Genetics knowledge was lowest at the oldest ages, among those with nursing diplomas as their highest education level, and among nurses. On multiple linear regression, significantly higher mean scores were found among those aged 30–49 years compared to respondents aged ≥50 years. Higher scores were also found for those with degrees and fellowships (except PhD) compared to those with nursing diplomas. Concerning cadre, general practitioners had significantly higher means compared to nurses as reference.
Table 3
Comparisons of genetics knowledge score by selected variables and regression analysis of healthcare practitioners as respondents in a survey within the Ibadan metropolis, Nigeria, 2018–2019 (N=415)
| Bivariable analysis* | Multivariable linear regression | ||||
|---|---|---|---|---|---|
| Variable | Mean knowledge score (SD) | n | p | β (95% CI) | p |
| Gender | |||||
| Male | 2.8 (1.0) | 159 | 0.002 | 0.09 (-0.16–0.34) | 0.467 |
| Female ® | 2.4 (1.0) | 256 | |||
| Age (years) | |||||
| <30 | 2.6 (1.0) | 63 | 0.025 | 0.29 (-0.10–0.69) | 0.140 |
| 30–39 | 2.7 (1.0) | 158 | 0.33 (0.03–0.63) | 0.033 | |
| 40–49 | 2.6 (1.1) | 100 | 0.36 (0.05–0.66) | 0.022 | |
| ≥50 ® | 2.3 (0.9) | 94 | |||
| Education level | |||||
| BSc/MBBS | 2.6 (1.1) | 301 | 0.002 | 0.51 (0.12–0.89) | 0.010 |
| Master’s degree | 2.7 (0.8) | 38 | 0.54 (0.04–1.04) | 0.033 | |
| Fellowship | 2.6 (0.6) | 33 | 0.60 (0.03–1.18) | 0.040 | |
| PhD | 2.7 (1.1) | 7 | 0.62 (-0.30–1.53) | 0.185 | |
| Diploma in nursing ® | 1.9 (0.8) | 36 | |||
| Specialty | |||||
| Internal medicine ® | 2.6 (1.0) | 96 | 0.757 | ||
| Pediatrics | 2.7 (0.8) | 29 | 0.19 (-0.26–0.63) | 0.417 | |
| Geriatrics/family medicine | 2.6 (1.1) | 63 | 0.12 (-0.23–0.46) | 0.514 | |
| Endocrinology | 2.2 (0.6) | 11 | -0.28 (-0.94–0.39) | 0.415 | |
| Obstetrics | 2.5 (1.1) | 58 | 0.22 (-0.14–0.57) | 0.240 | |
| Others | 2.5 (1.1) | 155 | 0.13 (-0.16–0.41) | 0.384 | |
| Cadre/designation | |||||
| Consultant | 2.7 (0.7) | 30 | <0.001 | 0.48 (-0.08–1.05) | 0.094 |
| Registrar | 2.7 (0.9) | 44 | 0.29 (-0.13–0.71) | 0.170 | |
| House officer | 2.8 (0.9) | 32 | 0.35 (-0.12–0.82) | 0.146 | |
| General practitioner | 2.8 (1.0) | 148 | 0.32 (0.04–0.60) | 0.025 | |
| Nurse ® | 2.3 (1.0) | 161 | |||
| % of DM patients among those managed | |||||
| <25 ® | 2.6 (1.0) | 250 | 0.350 | ||
| 25–49 | 2.6 (1.1) | 96 | 0.17 (-0.08–0.42) | 0.180 | |
| 50–74 | 2.3 (0.9) | 47 | -0.16 (-0.48–0.17) | 0.343 | |
| ≥75 | 2.6 (1.0) | 22 | 0.08 (-0.39–0.55) | 0.732 | |
Adequacy of training exposure to the use of genetic testing
Overall, younger (aged <40 years) HCPs perceived their training exposures to genetic testing as adequate, although the differences were not statistically significant between both age groups. Among the general population of HCPs interviewed, the majority had received training on obtaining comprehensive family pedigree (83.2%) and knew how often decision guidelines are needed (82.5%), while only very few (21.1%) had access to genetic testing services or had ever used a decision guideline algorithm (13.0%).
Perceived clinical utility of genetic testing
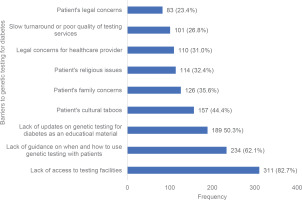
Overall, 360 (80.0%) perceived that genetic testing plays a central role in diabetes care, 174 (43.7%) had ever considered a diagnosis of MODY among their patients, while 136 (34.4%) had ever been responsible for treating a patient with a suspected diagnosis of MODY. The three topmost barriers to genetic testing in diabetic patients identified by participants were lack of access to testing facilities, lack of guidance on the use of genetic testing in patients, and lack of updates/educational materials on genetic testing in diabetes (82.7%, 62.1% and 50.3%, respectively) (Figure 1). Considering the cost-intensive nature of genetic testing for MODY, 138 (38.5%) HCPs perceived that genetic testing for MODY should be covered by insurance, while 60 (17.1%) supported insurance coverage only if the test outcome could change management or alter the progression of a patient’s condition.
DISCUSSION
Africa typically lags in accessing and benefiting from progress in medicine. At present, MODY is the only type of diabetes where patients’ outcomes in developed countries have been substantially impacted by advances in genomics. Findings from this survey uncover deficiencies in MODY-specific knowledge and application of genetics to diabetes care among the participating Nigerian HCPs, even though they recognized the importance of genetic testing in the management of diabetes patients. They also lacked confidence in their ability to identify and appropriately refer eligible diabetic patients for genetic testing. Finally, participants perceived a lack of access to genetic testing facilities and guidance on patients’ selection and referral as the foremost barriers to routine integration of testing into diabetes management. Amidst scant data from Africa, our study has highlighted what must be addressed for diabetes patients to take into account developments in the genomic revolution.
The mean MODY knowledge score was <2 out of a maximum of 9, and over 70% of respondents admitted to having very little or partial MODY knowledge. Age was significantly associated with the degree of MODY knowledge, with younger practitioners having relatively better MODY knowledge compared to older HCPs. Also, those practicing internal medicine and family medicine and working in public tertiary and secondary levels of care, had higher MODY scores. In a study involving 130 physicians, Haga et al.16 reported that the majority of primary care physicians rated their knowledge of basic genetic principles as high and scored high in the factual test as well. Van der Zwaag et al.14 sought the views of professional experts, including physicians from the Netherlands, specifically about MODY. Several participants perceived a lack of knowledge and awareness among HCPs as a significant barrier to requesting a genetic test for MODY. A qualitative study involving focus group discussions and key informants’ interviews (KII) on knowledge and attitudes to personal genomic testing for complex diseases in general was carried out in Nigeria17. The study, which included one doctor and one nurse to form a matrix from each health institution, reported that most participants in the KII showed limited knowledge of genomic testing. Like our study, the younger participants in this group displayed better knowledge. In contrast to our findings, the study by Alzu’bi et al.18 indicates that the majority of the 32 physicians they interviewed claimed they had, at least, a basic knowledge of genetics.
The reasons for the deficiency of MODY knowledge in our HCP respondents may have involved a challenge with the recall of already acquired knowledge of genetics during undergraduate training. In turn, recall may have been affected by low awareness and non-use of the knowledge. Perhaps, more realistically, a knowledge gap existed about MODY in the Nigerian undergraduate medical and nursing curricula. However, the relatively higher MODY scores demonstrated by the younger practitioners could be due to better exposure to developments in genomic knowledge in the training institutions and/or after graduation. Until recently, Nigerian medical undergraduates’ exposure to basic genetics was very minimal. However, in 2012, a new medical curriculum incorporating molecular biology and genetics as distinct courses was developed at the University of Ibadan19, adopted and recommended as a template by the Nigerian University Commission to other universities. Also, the relatively rare nature of MODY cases coupled with the need to confirm diagnosis by expensive genetic testing could have influenced our participants to be unmindful of MODY as a possible differential. The fact that some respondents had considered the possibility of MODY in their patients suggests the likelihood of undiagnosed MODY among Nigerians with diabetes. Measures need to be instituted to support HCPs to reduce the number of missed or misdiagnosed MODY cases.
As reported in other studies12,14, our participants also believed that genetic testing should play a central role in diabetes diagnosis, though they expressed limiting factors to its implementation. Consistent with the findings of previous workers15-17, and as viewed by most of our respondents, perhaps institutional training and education of HCPs in genetics was inadequate. Additionally, the lack of standard biomedical infrastructure and genomic expertise in services and research are known barriers to translational genomics in African countries. Fortunately, Africa has begun to receive support to address this situation, as exemplified in the H3 (Human Hereditary and Health) Africa project20 and the funding of this present study by Fogarty-NIH.
About half of the participants in our study believed there was no guidance on when and how to use genetic testing with diabetes patients and that updates on this information were not available as part of the ongoing educational experience. Most of the participants expressed the desire for some support tools that could aid the diagnosis of MODY, including clinical algorithms, helpful interactive websites, and consultation with experts. Indeed, there are freely accessible online training modules and podcasts (www.diabetesgenes.org and www.monogenicdiabetes.org) . Many authors and groups have proposed different supporting tools to improve the identification and selection of diabetes patients for MODY genetic testing. Such aids include practice guidelines, stepwise algorithms, web-based interactive platforms, and prediction calculators21-24. Algorithms are useful and needed in a setting such as developing countries with a greater need for cost consideration in the care of patients25-27.
Supporting African HCPs with diagnostic aids will improve their knowledge gap, reduce misdiagnosis and misclassification of MODY patients28, and allow diabetes patients to benefit from precision medicine29. Patients with HNF1A-MODY and HNF4A-MODY typically respond well to low-dose of sulfonylureas, while those with GCK-MODY do not require treatment with no consequence of later diabetes complications11,12,30. Patients with MODY and their families have expressed disappointment in the delay in making the right diagnosis occasioned by limited awareness and knowledge of physicians31.
Future directions and recommendations
Clearly, there is a need for larger studies both in urban and rural settings that cut across different ethno-geographic parts of a multi-ethnic country like Nigeria. Indeed, escalating similar studies to other parts of Nigeria will serve to further promote awareness of MODY among HCPs. Decision support aids, especially easily followed step-by-step contextualized clinical algorithms, are desirable to minimize misdiagnosis of MODY cases in Nigeria and the rest of Africa. Undergraduate medical and nursing curricula should reflect the current state of knowledge about genomics in general and its application to diabetes.
Strengths and limitations
The strength of this study is that we used a questionnaire developed by the authors following content and face validation by experts, including epidemiologists, diabetologists in Nigeria, and expert diabetologists in the US with experience in MODY care and research. The University of Chicago hosts the largest database on monogenic diabetes in the US. We were unable to find any previous reference of a validated questionnaire in the region that could be used to assess knowledge of HCPs on MODY, a condition with no existing data in Nigeria. There are some limitations in this study. Firstly, this study was carried out in only one city of Nigeria, Ibadan, albeit a major and densely populated city. The findings may be different in other regions of the country due to diverse ethnic and socio-cultural practices. Secondly, the study involved only doctors and nurses with the exclusion of other professionals in healthcare. However, doctors and nurses usually engage patients directly more than others in the hospital setting, even though their views may not be generalizable to other stakeholders in the healthcare sector. We are also aware that this was a crosssectional study. Finally, like any other survey, there could have been response bias between responders and nonresponders. However, we consider this to be minimal, given the high response rate (96%) in this study.
CONCLUSIONS
Basic MODY knowledge among Nigerian HCPs is unacceptably low. We have shown that the integration of genetic testing into routine diabetes care, as perceived by Nigerian HCPs, is challenged by deficient MODY-specific knowledge and clinical competencies, and barriers such as lack of access to genetic testing facilities and a useful support tool or aid. These factors must be addressed before the practice of precision diabetes medicine can be established in Nigeria and in the African continent. Failure to do so will further entrench persistent poor diabetes and patient-related outcomes in the continent.