INTRODUCTION
Most deaths (85%) from non-communicable diseases (NCDs) occur in low- and middle-income countries (LMICs)1. In Morocco, a lower middle-income country in the eastern Mediterranean, NCDs contributed to 80% mortality in 20162. Morocco has a population of 36.6 million, 73.6 years life expectancy at birth, 64.6% urbanization, and 73.8% are literate3. Globally, death from NCDs is mainly caused by cardiovascular diseases (CVD), cancers, respiratory diseases, and diabetes1. In Morocco, the mortality rate caused by CVD is 38%, with ischemic heart disease and stroke being the major causes of death (31.0% and 22.5%, respectively)4. Behavioral risk behaviors, such as smoking, hazardous alcohol use, sedentary behavior and unhealthy diets, significantly increase the risk of NCD mortality1. In the eastern Mediterranean region, the main CVD risk factors include tobacco use, hypertension, type 2 diabetes, physical inactivity, depression, and obesity5. In Morocco in 2000, the prevalence of hypertension was 33.6% and diabetes 6.6%6. Due to ageing, urbanization and globalization, the prevalence of multimorbidity (≥2 chronic conditions), have been increasing in LMICs7,8, including in the eastern Mediterranean region, and it is important to understand the local drivers of multimorbidity4. Against this backdrop, recent national community-based information on multimorbidity and its risk factors in Morocco are needed7,8.
Factors associated with multimorbidity include sociodemographic factors, such as being female8-10, older age8-10, lower education level10, lower socioeconomic status9, unemployed/retired10, and urban residence11. Multimorbidity behavior risk factors include obesity8,12, physical inactivity8,13, sedentary behavior14, alcohol consumption8,15, insufficient consumption of fruits and vegetables8, and tobacco use8,15. The study aimed to estimate the prevalence and associated factors of noncommunicable diseases multimorbidity among adults in Morocco.
METHODS
Sample and procedure
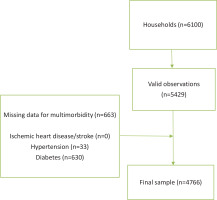
This is a secondary data analysis of the national cross-sectional Morocco STEPS 2017 survey16; the overall response rate to the study was 89.0%17. A multi-stage cluster sampling design was applied to generate representative data for adults aged ≥18 years in Morocco; more details elsewhere18. Men and women who were aged ≥18 years, resided in urban or rural areas, and were primarily living in regular households on the day of the survey met the inclusion criteria17. Exclusion criteria were people aged <18 years, people living in collective or nomadic households, people who were unable to answer questions, and those who had three unsuccessful visits within two days17. To account for non-responses, the sample size was multiplied by the inverse of the response rate, which was predicted to be 80%, yielding 6100 households17 (Figure 1); further details of the sample size calculation is found in the STEPS report17.
According to the STEPS survey procedures, Sociodemographic and behavioral information was collected by structured interview in Step 1. Physical measurements such as height, weight, and blood pressure were collected in Step 2. Biochemical measurements were collected to assess blood glucose in Step 316. The study was approved by the Biomedical Research Ethics Committee, Faculty of Medicine and Pharmacy of Rabat. Participants provided written informed consent17.
Measures
Outcome variable: multimorbidity
Diabetes was defined as fasting plasma glucose levels ≥7.0 mmol/L (≥126 mg/dL); or using insulin or oral hypoglycemic drugs19. Hypertension/raised blood pressure (BP) was based on measured blood pressure (average of two of last three measurements) and defined as systolic BP ≥140 mmHg and/or diastolic BP ≥90 mmHg or where the participant is currently on antihypertensive medication20. Ischemic heart disease/stroke was self-reported by response to the question: ‘Have you ever had a heart attack or chest pain from heart disease (angina) or a stroke (cerebrovascular accident or incident)?’ (yes, no)17.
From the three NCDs (diabetes, hypertension, and ischemic heart disease/stroke) a composite score was calculated, with ≥2 NCDs coded as 1 (multimorbidity) and ≤1 NCD as 08.
Behavioral NCD risk factors included past and current tobacco smoking (yes/no); current alcohol use (yes/no); low (<4 h/day), moderate (4 to <8 h/day) and high (≥8 h/day) sedentary behaviour21 based on the Global Physical Activity Questionnaire22; and inadequate fruit/vegetable consumption (<5 servings/day)17. Body mass index (BMI, kg/m2) based on measured height and weight was classified as: underweight (<18.5), normal (18.5–24.9), overweight (25.0–29.9), and obese (≥30.0)19. Sociodemographic information included education level, sex, age, and residence status17.
Statistical analysis
The STATA software version 15.0 software (Stata Corporation, College Station, TX, USA) was used for statistical analyses, taking multistage sampling and weighting of the data into account. Descriptive statistics (frequencies and percentages) are used to describe NCDs and multimorbidity. Univariable and multivariable logistic regressions were calculated on the associations between sociodemographic and health factors and multimorbidity using odds ratios and 95% confidence intervals. Variables significant (p<0.05) in univariable analyses were included in the multivariable models. A p<0.05 was considered significant.
RESULTS
Characteristics of the participants
The sample included 5429 people aged ≥18 years (mean age=45.1 years, SD=16.3), 50.9% were female, 64.1% lived in urban areas, and 36.4% had more than primary education. Slightly more than one in ten participants (11.6%) were current tobacco smokers, 1.7% current alcohol users, 76.3% had insufficient fruit and vegetables, 25.3% had low physical activity, 27.5% moderate (4 to <8 h/day) and 6.0% high (≥8 h/day) sedentary behavior, and 53.0% were overweight or obese (Table 1).
Table 1
Sociodemographic and lifestyle sample characteristics of community dwelling adults in the Morocco STEPS 2017 cross-sectional survey (N=5429)
Prevalence of diabetes, hypertension, ischemic heart disease/stroke and multimorbidity
The prevalence of diabetes was 10.7%, hypertension 19.5%, ischemic heart disease/stroke 3.3%, and multimorbidity 5.0%. Multimorbidity was highest among those aged ≥60 years (14.0%), those living in urban areas (6.1%) and those with obesity (9.1%) (Table 2).
Table 2
Distribution of diabetes, hypertension, ischemic heart disease/stroke and multimorbidity of community dwelling adults in the Morocco STEPS 2017 cross-sectional survey (N=5429)
Associations with multimorbidity
In the adjusted logistic regression model, older age (aged ≥50 years) (AOR=5.11; 95% CI: 3.64–7.18), urban residence (AOR=1.75; 95% CI: 1.26–2.43), moderate sedentary behavior (AOR=1.41; 95% CI: 1.08–1.85), being overweight (AOR=1.74; 95% CI: 1.21–2.49) and obese (AOR=2.34; 95% CI: 1.63–3.36) were positively associated with multimorbidity. More than primary education (AOR=0.67; 95% CI: 0.46–0.99), and high physical activity (AOR=0.70; 95% CI: 0.62–0.95) were negatively associated with multimorbidity. Furthermore, in the unadjusted analysis, male sex and current smoking were negatively associated with multimorbidity (Table 3).
Table 3
Associations between sociodemographic and behavioral factors with multimorbidity in community dwelling adults in the Morocco STEPS 2017 cross-sectional survey (N=4766)
| Variable | Categories | OR (95% CI) | AOR (95% CI)a |
|---|---|---|---|
| Age (years) | 18–49 ® | 1 | 1 |
| ≥50 | 6.17 (4.56–8.36)*** | 5.11 (3.64–7.18)*** | |
| Gender | Female ® | 1 | 1 |
| Male | 0.74 (0.56–0.97)* | 1.09 (0.77–1.54) | |
| Education level | None ® | 1 | 1 |
| Primary | 0.57 (0.40–0.82)** | 0.91 (0.61–1.36) | |
| >Primary | 0.38 (0.27–0.53)*** | 0.67 (0.46–0.99)* | |
| Residence | Rural ® | 1 | 1 |
| Urban | 1.90 (1.41–2.55)*** | 1.75 (1.26–2.43)*** | |
| Smoking status | Never ® | 1 | 1 |
| Past | 1.03 (0.65–1.65) | 0.84 (0.69–1.20) | |
| Current | 0.56 (0.33–0.95)* | 0.70 (0.38–1.31) | |
| Alcohol use | No ® | 1 | - |
| Current | 0.53 (0.13–2.23) | ||
| Fruit/vegetable intake (servings/day) | ≥5 ® | 1 | - |
| <5 | 0.82 (0.62–1.10) | ||
| Physical activity | Low ® | 1 | 1 |
| Moderate | 0.74 (0.53–1.03) | 0.84 (0.59–1.19) | |
| High | 0.44 (0.33–0.59)*** | 0.70 (0.62–0.95)* | |
| Sedentary behavior (h/day) | <4 ® | 1 | 1 |
| 4 to <8 | 1.77 (1.35–2.32)*** | 1.41 (1.08–1.85)* | |
| ≥8 | 1.69 (1.07–2.66)* | 1.03 (0.64–1.66) | |
| Body mass index | <25 kg/m2 ® | 1 | 1 |
| Overweight | 2.31 (1.63–3.26)*** | 1.74 (1.21–2.49)** | |
| Obese | 3.58 (2.53–5.07)*** | 2.34 (1.63–3.36)*** |
DISCUSSION
The study found in a national sample of adults (aged ≥18 years) in Morocco that 5.0% had multimorbidity (10.7% diabetes, 19.5% hypertension, and 3.3% ischemic heart disease/stroke), which is higher than in a national survey in Botswana (3.5% hypertension, diabetes and stroke/heart attack multimorbidity)8, but in a lower range compared to a review of studies in LMICs (3.2–90.5%)9. Compared to a national survey in Morocco 2000 (6.6% diabetes and 33.6% hypertension)6, the prevalence of diabetes (10.7%) increased and the prevalence of hypertension (19.5%) decreased in this 2017 study.
Consistent with previous findings8-11, we found that older age, female sex, lower education level, and urban residence, increased the odds of multimorbidity. Multimorbidity increases with age because of the cumulative effects of NCDs23. The higher rate of multimorbidity in women may be attributed to higher survival rates in women and higher utilization of healthcare associated with higher diagnoses rates in women compared to men9. In addition, women have a higher rate of being overweight/obese than men, which makes them more vulnerable to NCDs and multimorbidity8. Participants with better education may be more aware of health issues and subsequently engaged in a healthier lifestyle, which may prevent the development of NCDs and multimorbidity7.
In agreement with previous studies8,12-14, this survey showed that lifestyle factors (physical inactivity, sedentary behavior, and being overweight or obese) were associated with multimorbidity. While some previous research8,15 found an association between alcohol, tobacco use, and insufficient consumption of fruits and vegetable, and multimorbidity, we did not find any significant associations. Physical inactivity, sedentary behavior, and overweight and obesity can converge to increase vulnerability to NCDs and multimorbidity12. The proportion of people with inadequate physical activity in this study (25.3%) was higher than in a 2008 survey of Moroccan adults (16.5%)24. Similarly, the prevalence of being overweight/obese in this study (53.0%) was higher than in a 2008 survey of Moroccan adults (43.4%)25. This increase in NCD risk factors may increase multimorbidity. Population programs are needed to promote physical activity, a healthy diet, and body weight control in Morocco.
Strengths and limitations
The strength of the study is the nationally representative sample of adults in Morocco. Study limitations included the cross-sectional design which precludes causative inferences, and some self-reported data, which may have been biased. The variable on household income had too many missing cases and was therefore excluded from the analysis.
CONCLUSIONS
One in 20 adults in Morocco had multimorbidity and associated sociodemographic factors (older age, female sex, low education level and urban residence) and health factors (being overweight or obese, physical inactivity and moderate sedentary behavior) were identified that can help to plan interventions.