INTRODUCTION
Immunization of health workers (HWs) has become a top priority during the COVID-19 pandemic. According to the Centers for Disease Control and Prevention (CDC), ‘reducing the risk of patients catching influenza from health professionals, protecting healthcare staff and their families against influenza, and reducing health professionals’ absenteeism and consequently costs on the National Health Service’, are key reasons for the cost-effectiveness of influenza vaccination strategies among HWs1. Although the burden of influenza illnesses had declined in the COVID-19 era, the CDC reported that ‘9 million sick people, 4 million visits to a healthcare provider, 100000 hospitalizations, and 5000 deaths’ were attributed to influenza during the 2021–2022 season2. Throughout the COVID-19 pandemic, influenza vaccination coverage showed remarkable variation across nations (90% vs 24% in the US and Portugal, respectively)1. Therefore, it is plausible that vaccine hesitancy (VH) among HWs is one of the major hurdles to optimum immunization practices.
Despite the awareness amongst health professionals of the importance of immunization against infectious diseases, there are an array of factors and barriers to influenza vaccine uptake1,3. Vaccine hesitancy (VH) is defined here as ‘delay in acceptance or refusal of vaccines despite availability of vaccination services’, and exists on a continuous spectrum between complete refusal and complete acceptance3.This article investigates the impact of the COVID-19 pandemic on the sentiment of influenza vaccination among HWs. To do so, various determinants, barriers and interventions pertaining to vaccine hesitancy are identified. This scoping review is part of a broad project exploring vaccine hesitancy among health workers run by the World Federation of Public Health Associations (WFPHA)4.
METHODS
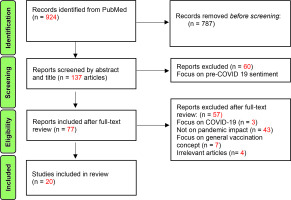
The aim of this scoping review was to examine the impact of the COVID-19 pandemic on HWs’ influenza vaccination sentiment. To do so, a literature search was conducted using the PubMed database, adopting a Boolean search strategy with the pertinent MeSH terms and keywords. These terms are provided in the Supplementary file Table 1. The search was restricted to articles in English that were original studies or meta-analyses or reviews, and published between August 2019 and July 2022. A PRISMA flow chart depicting the screening and selection process is shown in Figure 1.
Inclusion criteria were: articles had to focus on determinants, barriers or interventions for influenza vaccine hesitancy among health workers (HWs), during the COVID-19 pandemic. The studied population in the included articles was health workers, mainly in hospital settings.
Articles were excluded if: 1) they focused on the general population (or specific subgroups such as pregnant women) but listed HWs as a demographic characteristic, or exclusively focused on medical students; and 2) they were letters, correspondences, or editorials.
Abstracts and potentially relevant full texts for influenza studies were reviewed independently by two authors (RM, FG), with any conflicts resolved by consensus with the third author (ML).
RESULTS
Of the 924 articles screened, 20 studies met the inclusion criteria and were the final sample. Most studies were conducted in Europe (n=15). The majority were in Italy (n=7), followed by Poland (n=2), with Germany, Spain, Greece, Ireland, Cyprus, and Czech Republic one article each. Outside Europe, there was one study each from Iran, China, Lebanon, the United States and Saudi Arabia. There were 13 cross-sectional, 3 retrospective, 1 prospective, 1 prospective and retrospective, 1 comparative descriptive, and 1 predictive. Full details of the included articles are given in Table 1.
Table 1
Details of the included studies
| Authors Year | Country | Study design | Sample profession | Influenza season | Influenza vaccination rates during COVID-19 pandemic |
|---|---|---|---|---|---|
| Alharbi et al.19 2021 | Saudi Arabia | Cross-sectional | Physicians, pharmacists, nurses | 2019–2020 | 48.6% of participating HWs demonstrated adherence to seasonal influenza vaccination while almost 20.8% ‘never been previously vaccinated’. |
| Bertoni et al.6 2022 | Italy | Retrospective | Health personnel, administrative staff, technicians | 2018–2019 2019–2020 2020–2021 | Coinciding with the COVID-19 pandemic, the 2020–2021 season had the highest coverage (53.8%) of flu vaccine uptake, where males were two times and physicians were three times more likely to adhere to flu vaccination than their counterparts. This entails a 28.1% rise in 2020–2021 in comparison to the 2018–2019 season with health personnel (+36.1%) and technicians (+23.0%) showing the highest rise, unlike the administrative staff who showed a slight decline (-0.9% in 2020–2021 vs 42.4% in 2018–2019). For pharmacist and physician cadres, influenza immunization rates were stable throughout 2019 and 2020. |
| Collatuzzo et al.21 2021 | Italy | Retrospective | HWs | 2020–2021 2019–2020 | The COVID-19 vaccine hesitancy resulted in a higher ‘reporting of potentially adverse conditions (quantitative evidence of hesitancy of HWs) in the 2020–2021 flu campaign compared to the 2019–2020 one’, particularly among females and those aged 36–50 years ‘reported more often allergies’. |
| Costantino et al.11 2020 | Italy | Cross-sectional | HWs | 2019–2020 | In the 2019–2020 season, protecting patients was the chief reason for adherence to flu immunization among Sicilian HWs. The higher vaccination rates among younger HWs such as residents and trainees were attributed to high levels of awareness and confidence in influenza vaccine. The most significant reason reported was the fear of influenza vaccine-induced complications. Interestingly, positive perception and attitudes towards influenza vaccination among young health staff has influenced rise in older HWs’ flu vaccine uptake. |
| Di Giuseppe et al.10 2021 | Italy | Cross-sectional | HWs | 2020 | Influenza vaccine acceptance has increased during the COVID-19 pandemic where almost all (95%) and half (45.8%) of HWs who have been previously and never been vaccinated, respectively, reported willingness for influenza vaccine uptake in 2020–2021 season. |
| Di Pumpo et al.24 2021 | Italy | Predictive | Doctors, nursing staff, other healthcare workers, medical residents, administrative staff | 2019–2020 2020–2021 | The COVID-19 pandemic had a remarkable incentivizing effect increasing flu vaccine uptake (54.46%) among HWs during the 2020–2021 campaign. |
| Grochowska et al.8 2021 | Poland | Cross-sectional | Doctors, nurses, medical students, and other allied health professionals | 14 Sept. 2020 5 Nov. 2020 | 62.5% of HWs had higher trust rates in flu vaccines than in the COVID-19 one. However, 83.3% of HWs revealing willingness for flu vaccination (61.6%) also showed inclination towards COVID-19 vaccinations. Notably, acceptance towards flu immunization has doubled during 2020–2021 in comparison to 2019–2020 (61.6% vs 32.9%). On the other hand, 68.7% and 3.1% of participating HWs demonstrated willingness and complete refusal towards COVID-19 vaccine, respectively. Also, in comparison to non-HWs, the health staff are more accepting to COVID-19 vaccine. |
| Hajiabdolbaghi et al.23 2021 | Iran | Cross-sectional | HWs | 2019 | The ‘influenza mean vaccination coverage was 29.4%’ with difference in acceptance between males and females (35.85% vs 27.31%). |
| Jedrzejek and Mastalerz-Migas9 2022 | Poland | Cross-sectional | HWs | 2018–2019 2019–2020 | Flu vaccination coverage among both nurses (+7%) and physicians (+15.3%) had increased in the 2019–2020 season with a +13.3% rise in the overall vaccination coverage. |
| Kearns et al.18 2022 | Ireland | Cross-sectional | HWs, health administration | 2020–2021 | In 2020, 40% of the unvaccinated HWs at the 2019 flu campaign stated that the pandemic has positively shaped their attitude towards flu vaccines. Additionally, 94% of HWs plan to get a flu injection in 2020 in comparison to 78% of HWs vaccinated in 2019. The COVID-19 pandemic has boosted the adherence to influenza vaccine (28% and 27% agreed and strongly agreed, respectively, to receive flu vaccine ‘in light of COVID-19’). |
| Landwehr et al.13 2021 | United States | Comparative, Descriptive | Onsite employer-based health clinic | 2019–20 | 69% of participating HCs took influenza vaccination during the 2019–2020 flu season with a recognizable rise in vaccine adherence in comparison to the previous season of 2018–2019 (45 % vs 37%). |
| Papageorgiou et al.15 2022 | Cyprus | Cross-sectional | Private or public sector, either in primary or secondary health care services | 2019–20 | Influenza immunization coverage was 31.8% where the COVID-19 pandemic had an influential effect on 54.8%. The immunization rates were highest at ‘hospital Pediatric wards and ICUs’ (43.8 % and 38.2%, respectively). |
| Perrone et al.7 2021 | Italy | Prospective | HWs | 2020 | Awareness campaigns assisted in boosting influenza vaccine coverage among HWs (43.1% vs 21.5% in 2020 and 2019, respectively). Such campaigns covered the impact of vaccination to minimize health staff ‘absenteeism and disruption of health services, as well as in-hospital influenza outbreaks’. Physicians (mainly residents, ICU, and newborn health staff) and administrative staff embodied the most vaccinated cadre and surged immunization rates (308.3%) , respectively. |
| Rachiotis et al.17 2021 | Greece | Cross-sectional | Physicians, dentists, pharmacists | 2020–2021 | There was an enhancement in HWs’ flu vaccination rates (74%) mainly among physicians with the ‘acceptance of COVID-19 vaccination was the only predictor of influenza vaccination coverage’. |
| Redondo Marguello et al.14 2022 | Spain | Cross-sectional | General practitioners (GPs), primary care nurses | 2020 | The COVID-19 pandemic had surged the HWs’ awareness on immunization necessity where physicians and nurses showed ‘interest in’ getting ‘a range of internal and external information sources’ as well as attending ‘congresses, seminars or training activities of scientific societies’, respectively. Notably, previous flu vaccine adherence was high in the 2019 influenza campaign (78% of GPs and 85% of nurses). |
| Scardina et al.5 2021 | Italy | Retrospective | HWs | 2018–2019 2019–2020 2020–2021 | The COVID-19 pandemic has increased the positive HWs’ attitude (70.97%) towards flu vaccine given the fear from ‘co-circulation of influenza viruses and SARS-CoV-2’ where in 2020–2021, there was +230.6% (39.3%) rise in HWs’ flu vaccine coverage in comparison to 10.2% and 11.9% in 2018–2019 and 2019–2020 seasons, respectively. Notably, 10.6% of the participating HWs had higher acceptance rates towards influenza vaccine than COVID-19 one. |
| Stepanek et al.12 2021 | Czech Republic | Cross-sectional | HWs | 2019–2020 COVID-19 era | 57.9% of HWs had their first influenza vaccine injection during the COVID-19 pandemic when immunization demand was higher among physicians. And, the fear of mutual infection of flu and COVID-19 represented a strong driving factor. |
| Stockeler et al.22 2021 | Germany | Prospective and Retrospective | Emergency department personnel | 2016–2017 2020–2021 | In Germany, the 2020–2021 season was associated with higher vaccination adherence among emergency department personnel. Additionally, flu vaccine uptake was higher with the following factors: on-site vaccination, previous history of influenza vaccination adherence (at least twice), being a physician or a medical student in addition to acceptance towards COVID-19 vaccine. Interestingly, ‘self-reported vaccination coverage’ was almost doubled between 2016–2017 and 2020–2021 seasons (31% vs 59%). |
| Yi et al.16 2021 | China | Cross-sectional | HWs | 2019–2020 | In China, 67% was the flu vaccination coverage in the 2019–2020 season where 38.1%, 30.2%, 21.1%, 10.1% of which had ‘direct free’ immunization, workplace refund following vaccine uptake, self-funded and ‘health insurance reimbursement’, respectively. Accordingly, providing free vaccination was associated with higher HWs’ adherence towards flu vaccination (79% vs 34%). Also, mandatory (80%) and incentivized vaccination (70 %) had higher coverage than in workplaces ‘without any intervention measures (39%). |
| Youssef et al.20 2022 | Lebanon | Crosssectional | HWs | 2019–2020 2020–2021 | HWs showed high awareness (77%) along with high and moderate perception levels on the benefits of flu vaccination. Knowledge on vaccine’s safety made HWs 3.305 times more acceptable to get vaccinated than their counterparts. Boosting patients’ safety was the Lebanese HWs’ main perceived benefits for flu immunization (86.43%). However, safety doubts on flu immunization prevented 18.21% of Lebanese health staff from getting vaccinated. Additionally, 85.6% and 63.3% of Lebanese HWs showed concerns over governmental funding on vaccines believing that it should be offered for free besides concerns on a potential biased vaccine policy favoring the profit of drug companies, respectively. Eventually, 9.1% and 12.8% of Lebanese HWs revealed concerns on immune system overload and potential allergies, respectively. |
We analyzed a wide array of determinants, factors, barriers, and interventions for influenza vaccinations that were raised during the COVID-19 pandemic. Table 2 summarizes these for each country included in the review.
Table 2
Regional distribution of 4 general versus 24 specific aspects of influenza vaccine hesitancy determinants, enablers, barriers, and interventions among health workers
| General | Specific | Total | Country/Countries* |
|---|---|---|---|
| Determinants | Comorbidities | 4 | United States, Spain, Czech Republic, Cyprus |
| Age | 4 | Italy (n=3), Poland | |
| Gender | 4 | Italy | |
| Profession cadres | 7 | Italy (n=3), Poland, China, Czech Republic, Greece | |
| Vaccination history | 6 | Italy (n=3), Poland, Lebanon, Saudi Arabia | |
| Enablers | Health staff’s knowledge on influenza vaccine | 6 | Italy (n=2), Cyprus, Spain, Saudi Arabia, Lebanon |
| Concerns on self and others protection | 11 | Italy (n=3), Cyprus (n=2), Czech Republic, Poland (n=2), Ireland (n=2), Lebanon | |
| Rising perception of risk and fear from COVID-19 infection | 8 | Italy (n=5), Czech Republic (n=2), Poland | |
| Impact of influenza immunization | 4 | Italy (n=3), Lebanon | |
| Confidence in influenza vaccination | 6 | Italy, Poland, Ireland, Lebanon, Saudi Arabia, Iran | |
| Vaccine availability | 1 | Czech Republic | |
| Barriers | Negative perceptions about vaccine safety and effectiveness | 10 | Italy (n=4), Poland, Germany, Cyprus, Ireland, Saudi Arabia, Lebanon |
| Insufficient time for vaccine uptake | 8 | Italy, United States, China, Ireland, Poland, Spain, Cyprus, Iran | |
| Confidence in natural or acquired immunity | 9 | Italy (n=3), Ireland, Poland, China, Iran, Saudi Arabia, Lebanon | |
| Perspectives and attitudes towards vaccination | 2 | China, Iran | |
| Lack of knowledge about immunization | 2 | Italy, Lebanon | |
| Lack of trust | 2 | Poland, Lebanon | |
| Concerns on vaccine availability, cost, and needle injections | 5 | Italy, Poland, Ireland, Lebanon, Iran | |
| Interventions | Awareness campaigns | 12 | Italy (n=5), Poland, United States, Ireland, Germany, China, Czech Republic, Saudi Arabia |
| Targeting vaccine affordability and accessibility | 11 | Italy (n=4), United States, Germany, Ireland, Poland, China, Iran, Lebanon | |
| Education and training targeting vaccine hesitancy | 5 | Italy, Ireland, Spain, Saudi Arabia, Lebanon | |
| Mandatory HW influenza vaccination | 6 | Italy (n=2), Germany, China, Saudi Arabia, Lebanon | |
| Promoting vaccine culture in workplace | 6 | Italy (n=2), Ireland, Poland, Iran, Saudi Arabia | |
| Incentives approach | 4 | Italy, United States, Ireland, China |
Determinants of vaccine hesitancy
Evidence suggests the determinants of vaccine hesitancy among healthcare staff include age, gender, comorbidities, and profession cadres, in addition to vaccination history.
Age and gender
Evidence from Italy5-7, and Poland8 suggests the COVID-19 pandemic has positively influenced young HWs uptake of influenza vaccine. Italians aged <30 years showed an increased vaccination likelihood in 2019–20205 and Polish HWs aged 31–40 years had an increased immunization willingness in 2020–20218. This could be attributed to awareness campaigns, as well as the rising knowledge regarding the importance of influenza vaccination5.
There is consistent evidence among studies analyzed from Italy that males are more likely to accept influenza vaccination during the COVID-19 pandemic6,7,9,10. Young (25–35 years) male HWs demonstrated the biggest leap in vaccine adherence during the pandemic6, where Italian male healthcare staff had higher positive willingness toward flu immunization compared to females (74.7% vs 62.5%, respectively)10. However, Costantino et al.11 reported that ‘no significant differences’ exist between HWs’ genders.
Comorbidities
Evidence suggests that, in the context of the pandemic, healthcare staff with chronic diseases and comorbidities, defined here as hypertension, bronchial asthma, thyroid disorders, diabetes mellitus and rheumatic diseases, alongside sick HWs who are not on long-term medications12, have higher vaccine acceptance and flu immunization rates particularly in the US13, Spain14, Czech Republic12, and Cyprus15. This is evident in the Czech Republic, where flu immunization rates increased to 53.4% from 22.2%12. Comorbidities associated with a higher risk for flu complications ultimately act a positive prediction factor for influenza vaccination13. Redondo Marguello et al.14 noted that chronically ill HWs aged ≥65 years had a positive perception of flu vaccine effectiveness and benefits.
HWs’ profession cadres
Research shows there has been an increase of influenza vaccine uptake amongst healthcare staff, in particular those within intensive care units (ICUs), due to the COVID-19 pandemic, particularly in Italy6,7, China16, Czech Republic12, and Greece17. For example, in China ICUs had increased rates of flu vaccination among HWs compared to other units (70% versus 58%, respectively)16. This is further corroborated by Perrone et al.7 who noted how flu immunization rates were highest within the specialist medicine department, followed by specialist surgery, and administration departments (34%, 13.6 %, and 13.1%, respectively).
Moreover, in the context of the pandemic, physicians were found to be more willing to get vaccinated for influenza compared to nurses, mainly in Italy5,6, Poland9, Czech Republic12, Cyprus15, and Greece17. For example, in Cyprus, for the 2019–2020 season, physicians had higher influenza vaccination rates than nurses or other HWs cadres (68.9%, 20%, 29.8%, respectively)15. However, a recent cross-sectional study reported that nurses’ refusal rate to seasonal influenza vaccination has declined in the COVID-19 context12; amongst Italian nurses there was a 28.1% rise in influenza vaccination rate6. A similar rise can be seen among paramedical personnel, such as radiology and radiotherapy, but in regard to attitude towards vaccine uptake, with +30.3% reporting a positive attitude towards influenza vaccination during 2020–20216.
Non-physicians had a major concern of concomitant infection of influenza and COVID-19, specifically in Italy7 and Czech Republic12. This is evident in the +308.3% increase in participation among administrative staff, during the 2020 influenza vaccination campaign in Italy7. However, there are studies that suggest the contrary: the only noticeable decline in influenza vaccine uptake was among health administrators6,18. These studies showed a decrease of 3.2% in vaccination uptake among Italian administrative staff6, with Irish administrative staff reporting the lowest willingness for vaccination uptake18.
Vaccination history
There is evidence that the COVID-19 pandemic has increased the number of first-time influenza vaccine recipients particularly in Italy5,6 and Czech Republic12. For example, only 16% of the vaccinated Czech Republic HWs received seasonal influenza injections before the last season (2019–2020), and 25.2% of vaccinated Italian HWs got their first influenza vaccine in 2020–20216,12.
Healthcare staff adherence to influenza vaccination is associated with higher likelihood of influenza vaccination uptake amidst the COVID-19 pandemic particularly in Italy5,10,11, Poland9, Saudi Arabia19, and Lebanon20. Previously vaccinated HWs were 6 times more likely to get influenza vaccine than their counterparts20. Scardina et al.5 revealed that a recent history of influenza immunization is the utmost variable for predicting influenza vaccine acceptance, which is ‘correlated with a higher influenza vaccine attitude score’.
The COVID-19 pandemic had a critical impact on the success of influenza vaccination campaigns mainly in Italy5,6, Ireland18, and Lebanon20. The majority of Italian HWs in 2020–2021 declared the necessity of influenza vaccination at the time of COVID-19 pandemic5. However, Bertoni et al.6 mentioned that 28.6% of Italian HWs had maintained their positive influenza vaccination status during 2019–2020 and 2020–2021 seasons; only 11.5% of those previously vaccinated did not get vaccinated in 2020.
Enablers of vaccine acceptance
A wide array of factors affects acceptance of influenza vaccines by healthcare staff. These include: HWs’ knowledge of influenza vaccine (n=6), HWs’ concerns to protect others (family, friends, patients) (n=7), healthcare staff self-protection (n=4), increased perception of risk (n=5), increased fear of COVID-19 infection (n=3), reduction of the burden on healthcare systems (n=4), the role of public health professionals and health authorities (n=4), increased confidence in influenza vaccines in the COVID-19 context (n=6), and vaccine availability (n=1).
Knowledge of influenza vaccine
Research from Italy10,21, Cyprus15, Spain14, Saudi Arabia19 and Lebanon20 has shed light on HWs’ knowledge on influenza vaccine as a determinant of vaccine hesitancy. Due to the high risk of infection associated with their job, healthcare staff have more knowledge regarding influenza immunization21. For instance, Di Giuseppe et al.10 mentioned that 96.1% of Italian HWs had knowledge about influenza vaccines from reliable sources such as scientific journals (56.5%), Internet (25.3%), and colleagues (20.4%).
Concerns regarding protection
Studies highlighted that, in the context of the pandemic, HWs’ concerns to protect others (family, friends, and patients) acted as a major motivator for influenza vaccine acceptance. This was evident in Italy10,11, Cyprus15, Czech Republic12, Poland9, Ireland18, and Lebanon20. One study10 reported Italian healthcare staff’s sense of responsibility to prevent in-hospital spread of influenza in 2020. Another study18 noted how vaccinated Irish healthcare staff had concerns over family, patients, and colleagues’ protection.
HWs’ flu vaccination for self-protection was highlighted in four studies in Italy10, Poland9, Ireland18, and Cyprus15. In Italy, 81% of HWs reported self-protection as the reason for vaccination, with 98.1% in Poland, 79% in Ireland, and 77.4% in Cyprus9,10,15,19.
The protection of themselves and their family was a stronger motive for vaccine uptake amongst female compared to male HWs12,15. Male HWs noted that the main motivator was protecting patients, given their self-perception of the increased risk of catching influenza15.
Perception of risk and fear of COVID-19 infection
Increased perception of risk was reported in Italy5,6,10,11 and Czech Republic12. The COVID-19 pandemic was associated with a 50% increase in vaccination rates6, where the fear of spreading influenza was the main motivator for young HWs to get vaccinated12. Notably, HWs who have never been vaccinated reported less fear of influenza infection compared with those who have been vaccinated before10.
Evidence from Italy6, Poland8 and Czech Republic12 suggests the fear of COVID-19 infection had an influential effect on increasing the HWs’ acceptance of influenza immunization. The COVID-19 death toll contributed to the rise in influenza vaccine8. For example, 61% of Czech Republic HWs showed fear of having dual infections (influenza and COVID-19)12.
Impact of influenza immunization
The impact of influenza immunization to reduce the surge of cases as well as the burden on healthcare systems10 and decrease staff absenteeism11, has increased influenza vaccine uptake amongst motivated healthcare staff in Italy6,10,11 and Lebanon20. Approximately 80% of Lebanese HWs believed that influenza immunization would reduce ‘co-infection of influenza and COVID-19’, ultimately enabling ‘health services to better cope with COVID-19 complications’20, and thus limit confusion associated with the differential diagnosis influenza-like-illnesses6,10.
Confidence in vaccines
Public health professionals and health authorities have a critical role in boosting influenza vaccine adherence among healthcare staff particularly in Germany22, Cyprus15, Ireland18, and China16. For instance, 69% of vaccinated Irish healthcare staff found public health recommendations concerning influenza vaccine to be trustworthy18.
In the context of the pandemic, confidence in influenza vaccines has increased globally throughout Italy10, Poland8, Ireland18, Lebanon20, Saudi Arabia19, and Iran23; 66.3% of HWs deemed influenza a preventable infection, wherein concern (or lack thereof) regarding vaccine side effects acted as a predictor of willingness to vaccine uptake10. In Poland, Grochowska et al.8 stated that 62.5% of Polish HWs had increased confidence in influenza vaccination while 3.6% had more confidence in COVID-19 vaccines, and 26.3% trusted both vaccines equally. Eventually, 74.9%, 55.1%, and 53.3% of Italian HWs reported infection risk, vaccine effectiveness, and safety, respectively, for influenza vaccine adherence10.
Vaccine availability
Finally, policies securing on-site availability and convenient access to influenza vaccination are an important factor for vaccine adherence15,16,22, specifically, availability of vaccines in work settings. Stepanek et al.12 highlighted that Czech Republic HWs, especially those vaccinated in the 2019–20 season, had concerns on the shortage of influenza vaccines at their health facilities.
Barriers to vaccine acceptance
Evidence suggests that acceptance of influenza immunization is higher among healthcare staff with low perception of barriers to vaccination. In Lebanon20, acceptance was approximately 4 times higher amongst healthcare staff with low perception compared with others. Barriers to influenza vaccine among HWs include: false perceptions, doubts and misinformation about vaccine safety, adverse events, effectiveness; insufficient time for vaccine uptake; confidence in natural or acquired immunity from previous infections; HWs’ work expertise and peers’ perspectives and attitude towards vaccination; lack of HWs’ knowledge regarding immunization; lack of trust in healthcare organizations, health authorities, and pharmaceutical companies; and concerns on vaccine availability, costs and needle injections.
Negative perceptions regarding vaccinations
Negative perceptions are found globally, in Italy10,11,21,24, Poland (20%)9, Germany22, Cyprus15, Ireland18, Saudi Arabia (10.7%)22 and Lebanon20. In Germany, in 2020–2021, perceptions on influenza disease and potential immunization adverse effects varied significantly ‘between vaccinated and non-vaccinated Emergency Department personnel’22. A similar trend was seen among Irish HWs, wherein concerns regarding side effects due to the influenza vaccine varied from 2018 to 2020–2021 (65% vs 30%)18.
Safety doubts, alongside fear from influenza vaccine-induced complications were particularly important barriers to vaccine uptake in Italy11, Ireland (11%)18, Germany22 and Lebanon (18.21%)20. For instance, 9.1% and 12.8% of Lebanese healthcare staff revealed concerns regarding immune system overload alongside potential allergies, respectively20. However, it is important to note how all possible side effects due to influenza immunization, with the exception of injection pain, were higher among unvaccinated German HWs compared with their vaccinated counterparts for the 2020–2021 season22.
False perceptions pertaining to lack of vaccine effectiveness and efficacy were noted in Lebanon (7.86%)20, Ireland (21%)18, Cyprus (21.5%)15, Saudi Arabia19, and Iran (21%)23. In the Saudi Arabian study, 4% of HWs believed that influenza immunization could potentially cause influenza infection19. Moreover, confidence regarding influenza vaccine effectiveness was challenged due to perceptions of influenza as a non-dangerous ailment10,21,24.
Insufficient time for vaccine uptake
Vaccine accessibility, specifically lack of time to go and get vaccinated, was a barrier in Italy24, United States13, China (50%)16, Ireland (32%)18, Poland (30.4%)9, Spain14, Cyprus (3.4%)15, and Iran23, indicating that this barrier is widespread. In Spain, the study found that 62% of physicians and 72% of nurses were unable to prioritize preventative measures, such as influenza vaccination, due to the workload14. This sentiment is echoed by Yi et al.16 who highlighted that busy schedules were responsible for the lack of immunization against influenza amongst Chinese healthcare staff in high-risk departments.
Confidence in immunity from previous influenza infections
Confidence in natural or acquired immunity from previous influenza infections was noted as a barrier to vaccination in Italy10,11,24, Ireland (13%)18, Poland (17.8%)9, China (41%)16, Iran (33.8%)23, Saudi Arabia19, and Lebanon (22.8%)20. In Lebanon, 80.9% of healthcare staff regarded influenza as a mild infection, with additional few stating that the benefits of preventing influenza infection do not outweigh the barriers to vaccine acceptance and that immunization is not essential for healthy staff, 53.6% and 61.2%, respectively20.
Work expertise and peers’ perspectives
Work expertise and peers’ perspectives greatly influence HWs’ decision regarding influenza vaccine uptake in China16 and Iran23. The Iranian study found prior immunization experience, as well as negative feedback from non-vaccinated peers, ultimately enhanced HWs’ concerns regarding the development of side effects, in particular influenza-like symptoms23.
Knowledge about vaccination
Lack of healthcare staff’s knowledge about vaccination is a barrier to influenza vaccine acceptance in Italy10 and Lebanon20. In Lebanon, approximately 50% of HWs were not aware of the time frame for symptomology following exposure to influenza20. Additionally, around 24% of Lebanese HWs were uninformed of the possibility of immunization during active virus circulation20. Moreover, in Italy, approximately 54% of HWs were in need of further awareness of influenza immunization10.
Trust in organizations
Lack of trust in organizations or authorities, such as healthcare organizations, health authorities, or pharmaceutical companies, are an additional barrier to vaccine acceptance. This is particularly evident in Poland9 and Lebanon20. Nearly half of Lebanese HWs did not deem information from official authorities as reliable and had concerns regarding potentially biased vaccine policies that prioritize the profit of pharmaceutical companies20.
Vaccine availability
Evidence shows vaccine hesitancy is attributed to influenza vaccine availability, costs and needle injections in Italy5, Poland9, Ireland18, Lebanon20, and Iran23. Approximately 83% Lebanese and 25% Italian HWs reported concerns about insufficient vaccine availability, and unaffordable vaccine cost5,20. Irish HWs expressed an aversion to the influenza vaccination injection site, or preferred to avoid needle injections altogether23. Furthermore, nurses had more concerns regarding injections than physicians (10.7% vs 2.5%)9.
Barriers to influenza vaccine acceptance among HWs were common in all countries included in this review. A summary of enablers and barriers to vaccination are given Table 3.
Table 3
Distribution of 7 barriers versus 6 enablers to influenza vaccination among health workers across 20 of the included reference sources
| Barriers | Enablers |
|---|---|
| Negative perceptions about vaccine safety and effectiveness [9-11, 15, 18-23, 24] | Health staff’s knowledge on influenza vaccine [10, 14, 19-21] |
| Insufficient time for vaccine uptake [9, 13-16, 18, 23, 24] | Concerns on self and others protection [6, 8-12 15, 18, 20] |
| Confidence in natural or acquired immunity [9, 10, 11, 16, 18-20, 23, 24] | Perception of risk and fear from COVID-19 infection [5, 6, 10-12] |
| Work expertise and peers’ perspectives [16, 23] | Impact of influenza immunization [6, 10, 11, 20] |
| Lack of knowledge about immunization [10, 20] | Confidence in influenza vaccination [8, 10, 15, 16, 18-20, 22, 23] |
| Lack of trust in organizations [9, 20] | Vaccine availability [12, 15, 16, 22] |
| Concerns on vaccine availability, cost, and needle injections [5, 9, 18, 20, 23] |
Interventions for vaccine hesitancy
Interventions targeting influenza vaccine acceptance among HWs are ample and include: awareness campaigns, with dissemination of high-quality and transparent information on influenza vaccine, education and training targeting vaccine hesitancy; compulsory HWs’ influenza vaccination; promoting vaccine culture within workplaces; an incentives approach; and boosting vaccine affordability (defined as free-of-charge) and accessibility.
Awareness campaigns
Amidst the COVID-19 pandemic, awareness campaigns were the most popular intervention to increase influenza vaccine acceptance among HWs in Italy5-7,10,11, Poland8,9, United States13, Ireland18, Germany22, China16, Czech Republic12, and Saudi Arabia19. Educational messages included scientific-based information about the influenza vaccine, such as safety, efficacy, and pros and cons, as well as promotional educational material such as posters and flyers5,18.
Methods for awareness campaigns have extended to include compulsory sessions for HWs on influenza transmission18, implementing onsite influenza immunization promotion13, specific occupational counseling11, sending informative emails and reminders5, and running promotional events before seasonal campaigns19. This is in addition to the strategy of relying on the ‘hospital internal network’ to disseminate data on influenza vaccines12. Other methods to combat misconceptions regarding influenza vaccine are providing ‘educational handouts’ or arranging ‘lunch-and-learn activities’13.
Five studies discussed the importance of HWs’ education and training to reduce hesitancy towards influenza immunization in Italy5, Ireland18, Spain14, Saudi Arabia19, and Lebanon20. For instance, a broad range of ‘information sources’ as well as conducting ‘seminars or training activities of scientific societies’ were preferred by physicians and nurses, respectively14.
Mandatory vaccination
In the context of the pandemic, of all the strategies targeting vaccine uptake, mandatory influenza vaccination for healthcare staff was one of the most controversial in Italy10,11, Germany22, China16, Saudi Arabia19, and Lebanon20. However, evidence shows that vaccinated healthcare staff are more likely to favor compulsory influenza vaccine policies22. In China, 84% of HWs approved mandatory influenza immunization provided that the vaccination was free-of-charge and conveniently accessible16. On the other hand, in Germany, unvaccinated HWs were likely to agree that ‘mandatory vaccination policies would be a reason to change jobs’ as well as noting that ‘it would be ethical to not go to work during an influenza pandemic’22.
Vaccine culture within workplaces
Studies emphasized the importance of promoting influenza vaccine culture in different workplaces in Italy5,11, Ireland18, Poland9, Iran23, and Saudi Arabia19. This encompasses the increase of vaccine availability by making influenza vaccines free-of-charge19, the immunization of decision-makers and leaders as an approach for vaccine advocacy5,23, digital educational campaigns11, and managerial and peer pressure18. Evidence seems to suggest that positive perception and attitudes towards influenza vaccination among young healthcare staff leads to an increase in older HWs’ influenza vaccine uptake11.
Incentive approach
The incentive approach has also been utilized to increase influenza vaccine adherence in Italy7, the United States13, Ireland18, and China16. Incentives include cross-departments competition7, free-of-charge immunization13, or even vouchers18. For example, Chinese healthcare settings that incentivized influenza immunization among staff saw an increase in vaccine uptake (70% vs 39%, vaccine coverage among incentivized and non-incentivized, respectively)16.
Vaccine affordability and accessibility
In the COVID-19 context, evidence from Italy5,7,10,21, United States13, Germany22, Ireland18, Poland9, China16, Iran23, and Lebanon20 shows how vaccine affordability (defined as free-of-charge) and accessibility are instrumental for HWs’ immunization adherence. In China, free-of-charge vaccinations are likely to increase influenza immunization adherence by 45%; 79% vs 34% coverage in free-of-charge and non-free-of-charge vaccination policies, respectively16. Additionally, in Germany, it has been suggested that the increased influenza vaccination coverage among the emergency department’s healthcare staff, during 2020–2021, was attributed to the COVID-19 pandemic22. This is thought to be due to the increased availability of immunization clinics on-site22.
DISCUSSION
The purpose of this review was to summarize evidence regarding the impact of the COVID-19 pandemic on the sentiment surrounding influenza vaccination among HWs. To do so, various determinants, barriers, and interventions for vaccine hesitancy were identified.
Young HWs, specifically males, and HWs with chronic diseases and comorbidities, were associated with higher vaccine acceptance and influenza immunization rates. The pandemic has increased the uptake of influenza vaccination in different healthcare cadres, with physicians more willing to adhere to influenza vaccines. Furthermore, the number of first-time vaccine recipients has increased. However, previous adherence to influenza vaccination was associated with higher likelihood of up-taking influenza vaccination.
Interventions adopted during the COVID-19 pandemic to increase HWs’ influenza vaccine acceptance ranged from: awareness campaigns alongside education and training to target hesitancy; mandatory HWs’ influenza vaccination; promotion of vaccine culture in workplaces; the incentive approach; and increasing vaccine affordability and accessibility. Evidence suggests targeting and resolving myths surrounding the side effects of influenza vaccination lead to increased immunization adherence22. Thus, awareness campaigns should target negative perceptions regarding vaccination ultimately, and increasing trust in influenza immunizations16. Regarding training to reduce hesitancy, given the high cognitive awareness of healthcare staff, dissemination high-quality and transparent information was found to be crucial for effective promotion of influenza vaccine uptake. This is particularly important as, for example, in Italy, over half of HWs stated needing further awareness specific to influenza immunization10. Free-of-charge vaccines, alongside mandatory vaccination, achieved the highest vaccination coverage in China where 84% of HWs approved mandatory influenza immunization if vaccination is free and conveniently accessible16. However, regarding mandatory vaccination policies, given the varied success of this strategy, these are not applicable in all contexts10.
Factors that motivate healthcare staff acceptance towards influenza vaccines are abundant and directly related to: HWs’ knowledge on influenza vaccine; concerns to protect self and others; perceptions of risk; fear of COVID-19 infection; and confidence in health authorities. Notably, HWs have more knowledge regarding influenza immunization due to the nature of their profession. This could be attributed to the positive correlation between vaccine knowledge and ‘nationality, educational level, and perception’15,19. Moreover, concerns regarding protection (of others and themselves) were noted as an important factor, with HWs reporting a sense of responsibility to family, patients, and colleagues. Fear of spreading influenza, alongside the fear of COVID-19 infection, were determined to be a main motivator for HWs to get vaccinated. The belief that influenza immunization would ultimately reduce the co-infection of influenza and COVID-19, and, therefore, reduce the burden on healthcare systems, was a driving force for immunization.
There is consistent evidence that influenza immunization acceptance is 4 times higher among healthcare staff with low perception of barriers to vaccination20. Such barriers range from false perceptions and doubts about vaccine safety to confidence in immunity from previous infections. Regarding confidence in immunity, it has been noted that this sentiment could be attributed to healthcare staff belonging to an age group that has been reported to have a low perceived risk of catching influenza10,11.
Strengths and limitations
This review has limitations. First, it only included articles written in English. Nevertheless, there was a considerable number of publications on the topic of interest with the majority coming from non-English speaking countries. Thus, the studies included should be reasonably representative. Secondly, given the nature of the review (scoping, as opposed to systematic) – no quantitative analysis was performed, and we did not assess publication bias in the identified studies.
Nonetheless, strengths of the review lie in the narrative synthesis performed alongside identification of barriers. The latter can be addressed by policymakers in future pandemics.
CONCLUSIONS
This literature review showed that the COVID-19 pandemic had a critical impact on the success of influenza campaigns among HWs. Vaccine hesitancy among healthcare workers is a multifactorial phenomenon of utmost importance, especially during the times of a global pandemic. In the COVID-19 context, the confidence in influenza vaccines alongside the rising perception of risk have increased. A negative relationship between influenza immunization and COVID-19 infection was identified: the belief that the vaccine reduces co-infection of influenza and COVID-19, decreasing the burden on healthcare systems. The most effective intervention for increasing influenza vaccine acceptance among HWs was awareness campaigns as well as targeting vaccine affordability and accessibility. It is strongly recommended to conduct new empirical studies, particularly in low-middle income countries, to provide further evidence on the designated scope.