INTRODUCTION
Human papillomavirus (HPV) is a double-stranded DNA virus, which belongs to the family of Papillomaviridae1,2. There are over 100 types of HPV and they include HPV types 6, 11, 16, 18, 31, 33, 35, 39, and others3,4. However, about 30 HPV types are known to cause HPV-induced anogenital and oral infections5. These infectious HPVs are further categorized as ‘low risk’ and ‘high risk’ HPVs based on the clinical manifestations associated with the lesions they cause5. The low risk HPVs are responsible for causing benign epithelial hyperplasias (i.e. warts) while the high risk HPVs are responsible for causing malignant lesions (i.e. cancers)5,6-9.
The high risk HPVs are also called oncogenic HPVs. Oncogenic HPVs (such as HPV 16 and 18) are responsible for almost 100%, 90%, 70%, 50%, 40%, and 13–72% of cervical, anal, vaginal, penile, vulvar, and oropharyngeal cancers, respectively6-9,10-12. Every year, about 0.51 million women are newly diagnosed with invasive cervical cancer while 0.288 million women die as a result of the disease. Furthermore, approximately 80% of newly reported cervical cancer cases are from the developing world13. Similarly, about 30000 new cases of oropharyngeal cancers are reported yearly14.
There are various routes of transmission of HPV. The virus can be transmitted through sexual contact (e.g. anal sex, penetrative vaginal sex, and oral sex), skin-to-skin contact, and through child delivery (from mother to child)15-19.
The lifetime risk of HPV infection is as high as 80%20. Fortunately, HPV infection is a vaccine-preventable disease3. As a way of reducing the heavy burden of HPV-associated diseases among their populace, countries like Australia, USA, Norway, Austria, and Germany had included HPV vaccination programs into their routine immunization programs, years back21. Through massive vaccination campaigns against HPV, many people in these countries have been protected against HPV-associated diseases21. Unfortunately, in Nigeria, HPV vaccination is yet to be introduced into its national routine immunization programs despite the very high prevalence rate of HPV-associated diseases among its populace22,23.
Generally, young people are known to be a highly vulnerable population group when it comes to the risk of contracting HPV infections24-26. This assertion was made based on the rising rate of risky sexual behaviors (such as unprotected oral, vaginal and anal sexual intercourse) among the population group, coupled with the lack of a history of vaccination against HPV infection among them22,23,26.
In Nigeria, only very few and limited studies have assessed the knowledge of in-school young persons on HPV and HPV vaccines. Therefore, it will be of huge public health benefit if the prevalence and predictors of knowledge of young people in Nigeria on HPV and HPV vaccine are known, as such information will go a long way in helping the Nigerian government and other relevant stakeholders on how to develop, promote, and implement public health policies/ programs that will mitigate the community spread of the virus among them and also encourage their uptake of HPV vaccine.
This study was conducted with the aim of determining the prevalence and predictors of knowledge of senior secondary (high) school students (a population group that is predominantly made up of adolescents) in Nigeria on HPV and HPV vaccine. Conducting this kind of study amongst this population group is of high relevance because: 1) roughly 1 in 10 adolescents in Nigeria are sexually active27-32; 2) the knowledge of HPV and HPV vaccine among Nigerian adolescents reflects their collective level of preparedness towards the prevention of HPV transmission; and 3) the outcomes of this study will help to inform all relevant stakeholders in the Nigerian public health sector on how to effectively formulate, promote, and implement school health education policies/programs targeted at mitigating the spread of HPV infection among adolescents in Nigeria.
METHODS
Study design
This study was a descriptive cross-sectional populationbased study that was conducted in order to assess the level of knowledge of senior secondary school students in Nigeria on HPV and HPV vaccine. Also, this study forms part of the multi-year ‘Campaign for Head And Neck Cancer Education (CHANCE)’ Program conducted under the aegis of the Cephas Health Research Initiative Inc, Nigeria33-42.
Five geopolitical zones (south-west, south-south, northeast, north-west, and north-central), out of 6 geopolitical zones in Nigeria were randomly selected for the study. One state was randomly selected per zone, with the exception of the south-west zone where two states were selected. Using convenient sampling technique, a minimum of two schools were selected per state for the study. However, simple random sampling technique was used in the selection of the study participants. For a student to be considered eligible to participate in this study, he/she must belong to any of the senior classes (Senior Secondary Classes, SS1, SS2 and SS3) in a secondary school situated within Nigeria; and he/she must also be willing to participate.
Study instrument
The instrument used for the data collection was a selfadministered structured questionnaire that was developed through literature search43-49 and through a thorough review and editing process by a certified health education specialist (CHES). The questionnaire was anonymous and obtained information about sociodemographic characteristics (sex, age, tribe, religion, class, school etc.), knowledge of HPV, and knowledge of HPV vaccines from the participants.
Measures
Awareness of HPV and HPV vaccine
These were assessed using the questions: ‘Have you ever heard of the Human Papillomavirus (HPV)?’ and ‘Have you ever heard of HPV vaccine?’, respectively. The response options were ‘Yes’, ‘No’, or ‘I don't know’. Those that responded in the affirmative were considered as being aware of HPV and HPV vaccine, respectively.
Knowledge of HPV and HPV vaccine
Nineteen questions were used to assess knowledge of HPV among those participants who identified themselves to be aware of HPV, while five questions were used to assess the knowledge of HPV vaccine among those participants who identified themselves to be aware of HPV vaccine. The response options to virtually all these questions were ‘Yes’, ‘No’, or ‘I don't know’. Every correct response was given a score of ‘1’ and other responses were given a score of ‘0’. The total knowledge score on HPV and HPV vaccine was calculated for each participant, with the highest achievable score being ‘19’ and ‘5’ for HPV and HPV vaccine, respectively.
Data collection and entry
Between November 2016 and January 2018, a total of 3000 students who fulfilled the study’s eligibility criteria were approached for the study. They were informed about the purpose of the study. They were also informed that their participation is strictly voluntary and completely confidential. Only those students (2754) that agreed to participate and who also gave written informed consent were recruited and issued a self-administered questionnaire to fill in. A total of 2701 students returned their questionnaires to the investigators, giving a response rate of 98.1%. During the data cleaning process, 171 questionnaires were excluded from the study because a significant proportion of their content was inappropriately/not filled in. Finally, only 2530 filled questionnaires were considered for data analysis.
This study was conducted under strict compliance with the 1964 Helsinki Declaration on health research involving human subjects. Ethical clearance to conduct this study was obtained from the University of Ibadan, University College Hospital Institutional Review Board, Ibadan, Nigeria. Approval was also obtained from the participating schools. All participants were informed about the purpose of the study; they were also informed that their participation was completely voluntary and strictly confidential. Informed consent was obtained from the participants (i.e. SS1 to SS3 students), class teachers, and parents. All participation was voluntary. No participant was harmed as a result of the study.
Data analysis
Only the data obtained from the appropriately filled in questionnaires were analyzed using SPSS version 25 software. Frequency distribution of all variables was determined. The frequency distributions of all variables were obtained and the mean scores (and standard deviations) of the respondents’ age, knowledge of HPV, and HPV vaccine, were determined. Pearson’s chi-squared test was used to compare the sociodemographic characteristics of those respondents who were aware of HPV and HPV vaccine with their responses to the questions/statements assessing their knowledge on HPV and HPV vaccine, respectively. Also, those respondents who had average and/or above average scores on HPV and HPV vaccine were determined, classified and compared with the independent variables (sociodemographics) using Pearson’s chi-squared test. Multivariable logistic regression modeling was also done to determine the factors predicting the respondents’ knowledge of HPV and HPV vaccine. A p<0.05 was used to determine the level of statistical significance in the comparisons.
RESULTS
Sociodemographic data
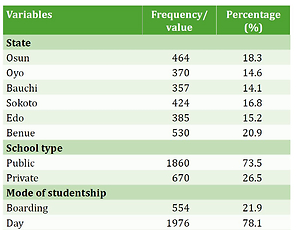
This study was conducted across six states, spreading across five geopolitical zones in Nigeria. One-fifth (20.9%) of the 2530 respondents were from Benue state (in the north-central zone of Nigeria). Their mean age (±SD) was 16.4 (±2.0) years, 56.0% were male, 34.9% belonged to the Yoruba tribe, 60.8% were Christians, 51.7% had monogamous family background, 73.5% were attending public schools, 78.1% were attending day-schools, and 31.3% were in SS1 (Table 1).
Table 1
Sociodemographic characteristics of respondents (N=2530)
Prevalence of awareness and knowledge of HPV and HPV vaccine
Only 23.0% and 18.3% of the respondents were aware of HPV and HPV vaccines, respectively (Supplementary file, Tables S1 and S2). Among those that were aware of HPV (n=583), the sources of their information were: TV/radio/ magazines (28.5%); internet (17.5%); health-workers (11.3%); friends (18.5%); and parents (10.6%) (Table S1). The majority (78.2%) of those who were aware of HPV had below-average knowledge score in their assessment on HPV (Table S1).
As for those who were aware of HPV vaccine (n=462), the sources of their information were: the internet (22.5%); school (18.4%); TV/radios (16.7%); health-workers (14.3%); posters in pharmacies (14.3%); student health centers (8.7%); information leaflets (6.1%); and other (4.3%). Their mean (±SD) knowledge score regarding their knowledge assessment on HPV vaccine was 1.0 (±1.2). The majority (74.0%) had below average knowledge about the HPV vaccine (Table S2).
Factors associated with awareness of HPV and HPV vaccine
Table 2 shows that a higher proportion of those respondents who were: aged ≥20 years (31.9%), from the Hausa tribe (27.4%); and attending private secondary schools (30.4%) were aware of HPV compared to: the adolescent respondents; those who were non-Hausas; and those attending public secondary schools, respectively (p<0.05).
Table 2
Sociodemographic factors associated with awareness of HPV and HPV vaccine, among those respondents that were aware of each one
| Variable | HPV | HPV vaccine | ||
|---|---|---|---|---|
| Yes* (%) | p# | Yes* (%) | p# | |
| Age (years) | 0.001 | 0.016 | ||
| Early adolescence (10–14) | 64 (17.2) | 51 (13.7) | ||
| Late adolescence | 467 (23.4) | 372 (18.6) | ||
| (14–19) | ||||
| Youth (≥20) | 44 (31.9) | 33 (23.9) | ||
| State | <0.001 | <0.001 | ||
| Osun | 93 (20.0) | 66 (14.2) | ||
| Oyo | 83 (22.4) | 60 (16.2) | ||
| Bauchi | 140 (39.2) | 119 (33.3) | ||
| Sokoto | 77 (18.2) | 83 (19.6) | ||
| Edo | 71 (18.4) | 50 (13.0) | ||
| Makurdi | 119 (22.5) | 84 (15.8) | ||
| Religion | 0.001 | <0.001 | ||
| Christianity | 315 (20.5) | 225 (14.6) | ||
| Islam | 254 (26.5) | 224 (23.4) | ||
| Tribe | 0.007 | <0.001 | ||
| Yoruba | 209 (23.6) | 144 (16.3) | ||
| Hausa | 164 (27.4) | 170 (28.4) | ||
| Igbo | 53 (21.2) | 38 (15.2) | ||
| Others | 157 (19.7) | 110 (13.8) | ||
| Type of school | <0.001 | <0.001 | ||
| Public | 379 (20.4) | 300 (16.1) | ||
| Private | 204 (30.4) | 162 (24.2) | ||
| School composition | <0.001 | <0.001 | ||
| Mixed | 381 (21.8) | 290 (16.6) | ||
| Boys only | 119 (21.6) | 110 (20.0) | ||
| Girls only | 83 (36.1) | 62 (27.0) | ||
| Class | <0.001 | <0.001 | ||
| SS1 | 140 (17.7) | 116 (14.7) | ||
| SS2 | 219 (26.4) | 179 (21.5) | ||
| SS3 | 195 (23.9) | 146 (17.9) | ||
Factors associated with knowledge of HPV and HPV vaccine
Table 3 shows that the respondents’ state of residence, tribe, and gender were significantly associated with their knowledge of HPV and HPV vaccine. In addition, the family background, religion, and school composition of the respondents were significantly associated with their knowledge of HPV vaccine.
Table 3
Sociodemographic factors associated with the knowledge of HPV and HPV vaccine, among those respondents that were aware of each one
| Variable | Average and above average score on HPV* (%) | p# | Above average score on HPV vaccine* (%) | p# |
|---|---|---|---|---|
| State | 0.002 | <0.001 | ||
| Osun | 30 (32.3) | 13 (19.7) | ||
| Oyo | 28 (33.7) | 12 (20.0) | ||
| Bauchi | 26 (18.6) | 43 (36.1) | ||
| Sokoto | 12 (15.6) | 32 (38.6) | ||
| Edo | 12 (16.9) | 10 (20.0) | ||
| Makurdi | 19 (16.0) | 10 (11.9) | ||
| Tribe | 0.020 | 0.008 | ||
| Yoruba | 60 (28.7) | 36 (25) | ||
| Hausa | 32 (19.5) | 58 (34.1) | ||
| Igbo | 10 (18.9) | 8 (21.1) | ||
| Others | 25 (15.9) | 18 (16.4) | ||
| Gender | 0.025 | <0.001 | ||
| Male | 83 (25.3) | 89 (34.2) | ||
| Female | 43 (17.5) | 29 (14.9) | ||
| Religion | 0.589 | 0.001 | ||
| Christianity | 66 (21.0) | 43 (19.1) | ||
| Islam | 58 (22.8) | 73 (32.6) | ||
| School composition | 0.277 | 0.005 | ||
| Girls only | 17 (20.5) | 6 (9.7) | ||
| Boys only | 20 (16.8) | 35 (31.8) | ||
| Mixed | 90 (23.6) | 79 (27.2) |
Factors predicting awareness and knowledge of HPV
We found that class, school composition, age, state (location of school), and tribe, were factors that predicted the likelihood of HPV awareness among our respondents (Table 4). For example, those respondents that were attending girlsonly (OR=2.86; 95% CI: 1.93–4.24) had the highest odds when compared with those attending other school types. Similarly, those in SS3 (OR=1.36; 95% CI: 1.00–1.84) had the highest odds when compared with those in other classes, while those schooling in Bauchi state (OR=2.56; 95% CI: 1.47–4.51) had the highest odds when compared with those schooling in other states.
Table 4
Predictors of respondents’ awareness of HPV and HPV vaccine
However, only gender and state were the factors that predicted a deeper understanding (knowledge) of HPV among our respondents (Table 5). Pertinently, the males were found to have higher odds (OR=1.76; 95% CI: 1.14–2.71) than females on the likelihood of having an average or above average knowledge score on HPV, while those schooling in Oyo state (OR=2.78; 95% CI: 1.05–7.34) had the highest odds of having an average or above average knowledge score on HPV when compared with those schooling in the other surveyed states.
Factors predicting awareness and knowledge of HPV vaccine
We found that class, school composition, age, state (location of school), and tribe were factors that predicted the likelihood of the respondents’ awareness on HPV vaccine (Table 4). For instance, those respondents that were attending a girls-only school (OR=2.80; 95% CI: 1.84–4.27) had the highest odds of being aware of the vaccine when compared with those from other school types, while schooling in Bauchi state (OR=2.87; 95% CI: 1.55–5.33) had the highest odds of respondents’ awareness on HPV vaccine when compared with those schooling in other states.
However, only family background, gender and state were the factors that predicted a deeper understanding (knowledge) of HPV vaccine among our respondents (Table 6). Furthermore, our findings showed that the males had higher odds (OR=2.89; 95% CI: 1.53–5.45) than females when it comes to having above average knowledge score on HPV vaccine knowledge assessment. Also, those respondents who were schooling in Sokoto state (OR=4.64; 95% CI: 1.32–16.28) or coming from a polygamous family (OR=1.83; 95% CI: 1.08–3.10) had higher odds than those in their counterpart groups (Table 6).
Table 6
Predictors of having an above average knowledge of HPV vaccine among respondents
DISCUSSION
This study surveyed 2530 secondary school students in Nigeria on their awareness and understanding of HPV and HPV vaccine and the findings are quite noteworthy.
Looking at the sociodemographic characteristics of the respondents, we observed that the study sample was very representative and diversified. The gender distribution of the surveyed respondents was fairly even. Also, all the three major Nigerian tribes (Yoruba, Hausa, and Igbo) were well represented in the study. However, the distribution of the respondents based on their religious faiths was skewed; only a very negligible number of our respondents who were practicing traditional religions participated in the study; this skewedness is expected because traditional religion is practiced only by a minority of Nigeria’s population50. Also, all forms of schools (such as boys-only, girls-only, mixed schools, private schools, public schools etc.) were included in the survey.
A large majority of the respondents were unaware of HPV and HPV vaccine. This finding is consistent with other published studies exploring awareness of HPV and HPV vaccine among Nigerian adolescents and young adults51-53. Furthermore, the generally low awareness rate of HPV and HPV vaccine in Nigeria is similar to that in high-income countries and other middle-income countries; this shows that low awareness rate on HPV and HPV vaccine among young persons is a global phenomenon, and not just limited to Nigeria54-57.
This study also shows that media and internet were the most commonly utilized sources of information on HPV and HPV vaccines among the respondents. This finding supports another study that reported that media and internet are top sources of information on HPV and HPV vaccine among high school students58. Also, the above confirm that media and internet are very powerful tools that can be judiciously used for disseminating information among Nigerian secondary school students, especially on issues pertaining to health. However, there are some other sources of information on HPV and HPV vaccine that were also utilized by the surveyed respondents. These sources include friends, parents, and health workers. However, this finding strengthens some Nigerian studies that reported that friends, health workers and parents can be a source of information on HPV and HPV vaccine41,59-62.
It is also noteworthy that many of those respondents who claimed awareness of HPV and HPV vaccines actually lacked adequate knowledge of HPV and HPV vaccines. This may suggest that their sources of information on HPV and HPV vaccine were probably inadequate or misleading; however, this suggestion is supported by previous studies, which reported that the quality of some health-related information shared among people, especially via the internet and social media, is unreliable63. This implies that all health-related information obtained from the internet and social media must first be scrutinized with extreme caution before its acceptance.
Also in this study, we observed that those respondents that belonged to a single sex (boys-only or girls-only) school, SS3 class, and a school located in Bauchi state, were more likely to be aware of HPV and HPV vaccine than their counterpart groups. These observations are very interesting, although not too surprising because: 1) most school-based health education programs in Nigeria are on reproductive health and commonly conducted at single-sex schools60; this may be a strong reason why students from single sex schools are more likely to be aware about HPV and HPV vaccines than those in mixed-sex schools; 2) The SS3 class is the highest level in the Nigerian senior secondary schools, nationwide; hence they are expected to be more knowledgeable than those in the junior classes due to their higher level of maturity and exposure to more information than the junior classes. However, based on the existing data and our knowledge of Bauchi state, we find it very difficult to explain how schooling in the state increases a student’s likelihood of awareness about HPV and HPV vaccine. Hence, this calls for future studies that will deeply explore this particular knowledge gap.
Interestingly, some factors were found to reduce the likelihood of the respondents’ awareness or understanding about HPV and HPV vaccine. Such factors include schooling in Sokoto state and having a polygamous family background. The reasons why those respondents in these categories had the likelihood of lacking knowledge or awareness about HPV and HPV vaccine cannot be ascertained based on the findings of the present study; hence, it will be worthwhile to conduct a study that will explore these area in the future.
However, it can be inferred from this study that many young in-school Nigerians are at high risk of developing HPV-associated diseases including HPV-induced cancers; this inference was made based on the observed low level of awareness of HPV and HPV vaccine among them. Unfortunately, among the infectious disease types ever known to man, HPV-induced cancers are among the notorious types13,14. Importantly, adequate knowledge about a disease goes a long way in the prevention of such disease60; if the youth in Nigeria are not made knowledgeable about HPV and preventive measures (such as HPV vaccination and the practice of safe sexual intercourse), then they stand a high risk of contracting HPV infections in the future.
Strengths and limitations
This study has limitations. This study adopted the use of convenience sampling technique (a non-probability sampling technique) in the selection of the schools that participated in the study; this gave all the schools in the participating states an unequal chance of participating in the study. Also, not all the states in Nigeria were included in the study due to limited financial and human resources.
Notwithstanding the limitations, this study is believed to be the largest survey assessing the knowledge of HPV and HPV vaccines among senior secondary school students in Nigeria. Furthermore, this study was conducted at a period when the Nigerian government is yet to introduce HPV vaccination into the national immunization programs in Nigeria22,23. Hence, the findings obtained in this study will provide additional relevant information to the government and all other relevant stakeholders towards the formulation and implementation of HPV sensitization and immunization policies and programs in Nigeria.
Recommendations
Based on our findings and our discussion so far, we make the following recommendations. First, a nationally representative study that will determine the prevalence of risks of contracting HPV infection (such as unprotected sexual intercourse, sexual violence etc.) among in-school youth in Nigeria needs to be conducted. Second, a nationwide school-based campaign/sensitization on HPV prevention (with focus on HPV-induced cancers) among young people in Nigeria needs to be conducted. Third, the Federal Government of Nigeria needs to quickly introduce HPV vaccine into the routine immunization program of Nigeria to curb the spread of HPV infection in Nigeria.