INTRODUCTION
Tobacco consumption results in illnesses and has been implicated to be a significant risk factor for many chronic non-communicable diseases including cancers, cardiovascular diseases, chronic obstructive pulmonary diseases (including emphysema and chronic bronchitis), lung diseases, stroke, and diabetes, among other diseases1-3. In 2019 alone, tobacco use accounted for approximately 200 million Disability Adjusted Life Years and caused about 7.65 million deaths globally4,5. According to the World Health Organization (WHO), tobacco kills more than 8 million people every year and of this about 15% is due to exposure to secondhand smoke1,6,7. In addition, studies have shown that the healthy life expectancy of smokers is 5–10 years lower relative to that of non-smokers8. When compared with other modifiable risk factors for many diseases, tobacco consumption remains the leading preventable cause of morbidity and mortality globally9-11.
In recent years, the prevalence of tobacco consumption has declined around the world, especially in developed countries12. Nonetheless, about 22.3 % of the world’s population, 36% of all males and 7.8 % of all females, were tobacco users in the year 2020 and of this global burden of smoking more than 80% of 1.3 billion tobacco users live in low- and middle-income countries (LMICs)13. This is despite the fact that LMICs bear a disproportionate burden of non-communicable diseases as well as the consequent economic burden14-16. In Sub-Saharan Africa (SSA), the prevalence of current tobacco use is substantial. A study conducted in four SSA countries among adults aged 40–60 years, revealed that, on average, about 34.5 % of men and 2.1% of women sampled in the study were current smokers17. Another study carried out among a larger sample of SSA countries showed that the prevalence of current tobacco use ranged between 6.1% in Ghana to 38.6% in Lesotho18. In absolute terms, this represents a huge number of tobacco users, and hence an enormous macro- and micro-economic burden due to tobacco consumption in SSA.
Essentially, the burden of tobacco use further complicates the fragile health systems in SSA in terms of the triple burden of emerging and re-emerging infectious diseases, non-communicable diseases, and the fiscal constraint that is currently facing health systems in the region. Many countries in SSA allocate extremely insufficient financial resources for the provision of healthcare services, which are the lowest relative to the financial resources available for healthcare provision in other regions of the world. According to the data published in the WHO Global Health Expenditure Database, average health expenditure declined from 5.3% of the total gross domestic product (GDP) in the year 2016 to 4.9 % in 2019 in SSA19. This is far below the 12% of total GDP recommended by the WHO20 and even lower than the proposed 15% of government expenditure, jointly agreed by members of the African Union at the Abuja declaration more two decades ago21.
As in many SSA countries, tobacco consumption remains a public health issue in Nigeria, with implications for population health and the economy. A systematic review and meta-analysis of the burden of current tobacco use in Nigeria reported that the prevalence of current tobacco consumption and ever tobacco use were 10.4% and 17.7%, respectively, between 1995 and 201520. This translates to more than 11 million smokers within that period, which is concerning considering the health effects of tobacco use on public health and its consequent impact on government spending on healthcare services as a result of illnesses caused by tobacco use.
Studies have shown that the economic burden of tobacco consumption can be felt at individual, household, organizational, and at societal levels22. Some of the economic consequences include its effect on the consumption budgets of poor individuals and households, its effects in terms of direct spending towards purchasing tobacco products, direct and indirect expenditures to access healthcare services due to tobacco-induced diseases, productivity losses for firms, its impact on government aggregate health expenditures, etc. In recent years, there has been some progress with tobacco control activities in Nigeria. However, these efforts will further benefit from evidence-based findings in terms of the magnitude of the economic burden of tobacco consumption in the country. Currently, the extent of the tobacco problem has not been matched by research and thus this study aimed to estimate the economic burden of tobacco consumption in Nigeria. Findings from this study will be beneficial as an input into the cost-effectiveness analysis of public investment toward controlling tobacco use in the country.
METHODS
A prevalence-based risk attributable fraction23 and human capital approaches24 were used to estimate the economic burden of tobacco consumption for the years 2013–2020, in Nigeria. There are 2 components of the economic burden of tobacco use estimated in this study. First, the direct cost was estimated by ascertaining the proportion of aggregate health expenditure categories attributable to tobacco consumption. Secondly, the indirect cost due to morbidity and mortality as a result of tobacco-related illnesses was estimated and this was aggregated together with the direct costs estimated in the first step. For the first component, aggregate health expenditure categories related to non-communicable diseases reported for Nigeria were from the WHO Global Health Expenditure Database19. The expenditure categories included current health expenditure, domestic general government health expenditure, external sources of funding, domestic private health expenditure, and capital health expenditure. All expenditure categories were reported in US$. The attributable fraction was applied to these expenditure categories to see what proportion of the expenditure categories were attributable to tobacco consumption during the period of analysis. However, emphasis was placed on current health expenditure since it captured other categories of aggregate expenditure. Data on the prevalence of current and ever tobacco use were from the Global Adult Tobacco Survey (GATS)25 implemented in 2018 in Nigeria and from a study on the prevalence of current and ever tobacco use in Nigeria26. The all causes, all ages, and relative risks of mortality due to smoked and smokeless tobacco use among males and females reported in another study were utilized27. Data on the labor participation rate, national minimum wage, a life table (the probability of mortality), and the Nigerian population and the GDP for the years under review were from the WHO Global Health Observatory data repository and the World Bank data repository23.
For parsimony and to ensure that the estimated economic burden of tobacco use is as accurate as possible, only aggregate expenditures related to non-communicable diseases (NCDs) were included in the estimation. This is plausible because tobacco use has been reported as being a major risk factor for most NCDs12. Also, the estimation of the economic burden of morbidity and mortality attributable to tobacco consumption was assumed to have occurred among people aged 25–54 years. The rationale for this is the reported time lag between tobacco initiation and when the health effects fully begin to manifest themselves and also considering that the average life expectancy in Nigeria is 53 years, according to World Bank data28.
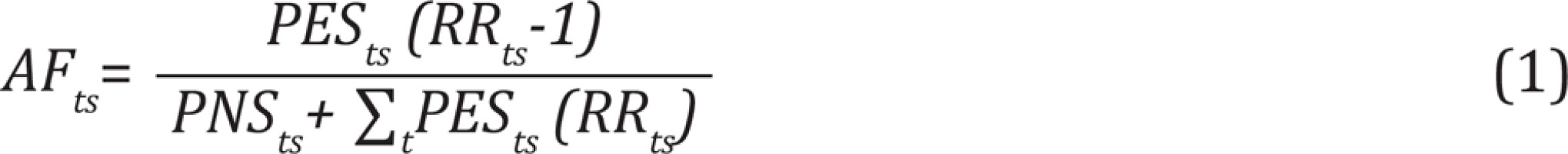
Estimation of attributable fraction due to tobacco use
The estimation of the economic burden of tobacco consumption in this study is methodologically straightforward forward and a critical part of this is the adoption of the attributable fraction (AF) strategy. The proportion of reported aggregate expenditure categories as well as the reported level of morbidity and mortality that are attributable to tobacco use were estimated using the AF which was calculated as follows:
where AFts denotes the attributable fraction by type of tobacco use t (smoked or smokeless tobacco use) and sex s (males or females), PES refers to the prevalence of ever smokers, PNS refers to the prevalence of never smokers, and RR is the all cause, all ages relative risk of morbidity and mortality due tobacco use.
Estimation of direct costs and the indirect costs of morbidity and mortality attributable to tobacco consumption
The estimated AFts was applied to the data on aggregate expenditure categories to ascertain the proportion of the expenditure categories that were attributable to tobacco consumption during the period under review. To estimate the morbidity and mortality costs attributable to tobacco use, the following steps were followed:
Step 1: Estimate the number of unemployed population among males and females, 2013–2020, by multiplying the total population of males and females aged 25–54 years by the reported labor participation rate among males and females during that period and subtract this from the total population of males and females aged 25–54 years. This is described in the equation below:
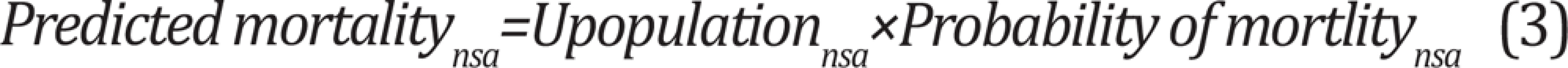
where Upopulationnsa is the number of unemployed population by year n, sex s and age group a, i.e. the population aged 25–54 years which forms the labor force of the country. Although, the average age of retirement in Nigeria is 60 years, the analysis used ages 25–54 years considering that the average life expectancy in Nigeria is 53 years, as noted earlier.
Step 2: Predict the probability of mortality among the unemployed labor force by multiplying the number of unemployed individuals, males, and females, aged 25–54 years, by the probability of dying within those ages using the probabilities reported in the WHO life table for Nigeria. The intuition behind this is that while what is calculated could have been mortality from any cause, morbidity and mortality prevents people from labor participation, and the proportion of this attributable to tobacco use is retrieved in Step 4.
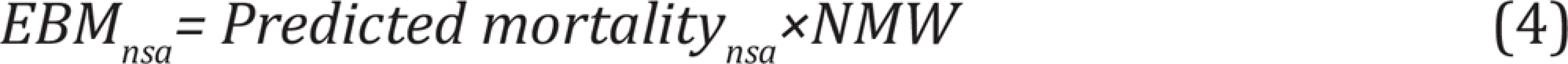
Step 3: Determine the economic burden of mortality (EBMnsa) from all causes among males and females, among people aged 25–54 years, by multiplying the predicted mortality (i.e. all causes mortality) among the male and female population by the annual average national minimum wage (NMW).
Step 4: Isolate the economic burden of mortality and morbidity attributable to tobacco consumption (EBMnsa) by multiplying the all causes economic burden of mortality by the estimated AF.
Since there are no reported relative risks of morbidity among smokers relative to non-smokers for Nigeria, the estimated EBMnsa×AFts was multiplied by 2 to capture the economic burden of morbidity due to tobacco use following a similar approach used in a previous study23.
RESULTS
The expenditure categories for the years 2013 to 2020 are reported in Table 1. In 2013, current health expenditure was $17.62 billion and increased to $19.04 billion in 2014. However, it dropped in 2015 to $17.72 billion. There was a further decrease the following year when it dropped to $14.76 billion but it remained fairly stable between 2016 and 2020. Other expenditure categories had different patterns in terms of yearly values. Across all the years, current health expenditure was the largest, followed by domestic private health expenditure and external sources of funding were the lowest. Between 2013 and 2020, the total current health expenditure on non-communicable diseases in Nigeria was $124.95 billion. The share of current health expenditure on non-communicable diseases as percent of GDP was the highest between 2015 and 2017 at 4% in those years. On average, only 3% of the GDP was spent on NCDs in Nigeria for the entire period. Between 2013 and 2020, domestic general government health expenditure on NCDs, external sources of funding on NCDs and domestic private health expenditure on NCDs followed a similar pattern. However, capital health expenditure was the highest in 2013 ($1.2 billion) and in 2018 ($1.1 billion).
Table 1
Summary of categories of aggregate health expenditure in Nigeria (2013–2020)
Table 2 shows the all cause, all ages relative risk (RR), the prevalence of smoked and smokeless tobacco use, and the estimated attributable fraction. The reported prevalence of ever and current smoked tobacco use was 17.7% among males and 1.93% among females in Nigeria. For smokeless tobacco, 2.9% of males and 0.9% of females were ever and current smokeless tobacco users. The relative risk of mortality among tobacco users relative to non-users was 1.55% higher risk for male smokers and 1.40% higher risk for female smokers. For smokeless tobacco, males were at a higher risk of mortality by 1.16% compared to non-smokeless tobacco users while females who use smokeless tobacco were at a higher risk of mortality by 1.25% relative to those who do not use smokeless tobacco. Of the total economic burden of non-communicable diseases, 0.07% was attributable to smoked tobacco use and 0.004% attributable to smokeless tobacco among males, while for females it was 0.005% for smoked and 0.002% for smokeless tobacco use, in Nigeria.
Table 2
All-cause, all ages relative risk, the prevalence of tobacco use, and attributable fraction
[i] It was assumed that the prevalence of tobacco use remained the same during the period when the economic burden of tobacco use was estimated. The all-cause, all ages relative risk reported in Gupta et al.27 were adopted to calculate the same for Nigeria.
Table 3 shows the direct component of the economic burden of tobacco consumption for the years 2013–2020 by sex and by expenditure categories, in Nigeria. Across all the years, the economic burden attributable to tobacco consumption was higher among males compared to females. For current health expenditure category and among males, the economic burden attributable to smoked tobacco use was the highest in 2014 at $1.33 billion and was the lowest in 2018 at $912.42 million. Also, it was the highest in 2014 for females at $95.18 million. Between 2013 and 2020, the total direct cost attributable to smoked tobacco use among males and females for current health expenditure was $9.37 billion, and $749.66 million for smokeless tobacco. Combined, the economic cost attributable to tobacco use between 2013 and 2020 was $9.45 billion.
Table 3
The economic burden attributable to tobacco consumption by sex and yearly health expenditure categories in Nigeria (2013–2020)
[i] The rows denote the following yearly expenditure categories: Current health expenditure; Domestic general government health expenditure; External sources of funding; Domestic private health expenditure; Capital health expenditure. All values are in million US$. The total economic burden attributable to tobacco use summed only the totals for current health expenditure for both smoked and smokeless tobacco.
The economic burden of morbidity and mortality attributable to smoked and smokeless tobacco use by sex and age group between 2013 and 2020 is shown in Table 4. In terms of the total values, the economic burden attributable to smoked tobacco use was the highest among males aged 50–54 years, $8.04 million, and the lowest among males aged 25–29 years, $4.65 million. The pattern was the same for smokeless tobacco with the total economic burden attributable to smokeless tobacco use being $265820.66 among males aged 25–29 years and $459463.02 for those aged 50–54 years. For female tobacco users, the economic burden of morbidity and mortality attributable to tobacco use showed no particular pattern. The estimated economic burden of morbidity and mortality from smoked tobacco use for females was the highest among those aged 30–34 years ($518195.43) and the lowest among those aged 40–44 years ($272496.15). Combining the values for males and females and for all age groups, the total indirect cost of morbidity and mortality attributable to both smoked and smokeless tobacco use was $ 45966085.49 for the period between 2013 and 2020.
Table 4
Economic burden of morbidity and mortality attributable to tobacco use by sex and age group (2013–2020)
Table 5 shows the annual GDP, the estimated economic burden of tobacco consumption and its proportion to GDP, for the years 2013–2020. The economic burden attributable to tobacco consumption was the highest in 2014 at $1.55 billion and was the lowest in 2018 at $1.06 billion. In 2017, the economic burden of tobacco consumption as a proportion of GDP was 0.31%, which was the highest across the years. The lowest economic burden attributable to tobacco consumption was 0.26% of GDP in 2019. On average, the economic burden attributable to tobacco use was 0.28% of GPD between 2013 and 2020, in Nigeria.
Table 5
Yearly GDP and economic burden of tobacco consumption (2013–2020)
DISCUSSION
Using a prevalence-based risk attributable approach, this study estimated the economic burden of tobacco consumption in Nigeria between 2013 and 2020. This represents an attempt to estimate the cost burden of tobacco use from a macro-economic perspective in Nigeria. Although earlier studies had estimated the economic burden of tobacco use, using a micro-economic approach29,30, this study takes a holistic view by including aggregate expenditure categories related to non-communicable diseases including current health expenditures, domestic general government health expenditure, external sources of funding, domestic private health expenditure, capital health expenditure as well as using the human capital approach to assess the economic burden of morbidity and mortality attributable to tobacco consumption in Nigeria.
The attributable fractions estimated in this study were 0.07% and 0.004% for smoked and smokeless tobacco use, respectively, among males. Among females, the estimated attributable fractions were 0.005% for smoked tobacco and 0.002% for smokeless tobacco use. These estimates are smaller compared with those reported in previous studies. A study implemented to investigate the economic burden of tobacco use in India reported attributable fractions of 18.15% for smoked tobacco use and 3.71% for smokeless tobacco use, among males aged 35–69 years, and 1.95% and 5.30%, respectively, for females aged 35–69 years23. A review of different techniques for estimating attributable fraction revealed that globally, morbidity and mortality attributable to tobacco use ranged from 8% in Southern Africa to about 35% in Hong Kong, among male and female populations31. The huge difference between the attributable fractions reported in earlier studies and those reported in this study is not surprising because the magnitude of the estimates is always a function of the prevalence of ever and current tobacco use which is much lower in Nigeria compared to many other countries. Nonetheless, the attributable fractions reported in this study represented a significant portion of the economic burden of non-communicable diseases and the consequent morbidity and mortality in Nigeria.
The estimated direct economic cost attributable to tobacco consumption in this study was $9.41 billion between 2013 and 2020. This represents a proportion of the total current health expenditures on non-communicable diseases for the period under review. Using total current health expenditure due to all causes would have significantly increased the estimates in terms of the economic burden of tobacco consumption but doing so could lead to an upward bias in the estimated value. Even though the adverse outcome of infectious diseases could be aggravated by tobacco use, it is more of a risk factor for NCDs relative to non-communicable diseases. This assertion is corroborated by a study that estimated the macro-economic burden of NCDs attributable to tobacco use in China. The study projected that tobacco attributable NCDs will impose about $2.3 trillion between 2015 and 2030 in China32. The value of the estimated economic burden attributable to tobacco consumption reported in Chen et. al.23 is higher than that reported in the present study for obvious reasons including the longer duration of the projection, the higher rates of ever and current tobacco use, and the huge population of China. Moreover, better quality of care has been liked with higher healthcare costs as healthcare services are often more expensive in advanced healthcare settings relative to what is obtainable in LMICs. Hence, this could be a determining factor in terms of the magnitude of the economic burden of tobacco consumption reported in high income countries compared with developing countries.
Similarly, the indirect cost estimated in this study was $45.5 million during 2013–2020, which is well below what has been reported in previous studies. For instance, a study reported that the proportion of indirect cost as a percentage of the total economic burden of tobacco use was 78%. Furthermore, this study revealed that between 2013 and 2020, tobacco related NCDs imposed a total of $9.45 billion on the Nigerian economy, with an average of $1.27 billion annually. This finding is comparable to the findings reported in an earlier study in Nigeria. A previous study carried out to estimate the health and economic burden in Nigeria reported that in 2019 alone, the economic burden attributable to tobacco consumption was $1.71 billion, which is slightly higher than in this study. However, findings from similar studies conducted in countries where the prevalence of tobacco use is higher than in Nigeria, reported a much higher economic burden of tobacco use. For instance, a study conducted in India revealed that tobacco use imposed approximately $27.5 billion on the country’s health system between 2017 and 201823. Similarly, a study that investigated the health and economic burden of tobacco use in 12 Latin American countries (Argentina, Bolivia, Brazil, Chile, Colombia, Costa Rica, Ecuador, Honduras, Mexico, Paraguay, Peru, Uruguay), revealed that tobacco use is responsible for over $26.9 billion annually, in those countries33. These findings show that the overall impact of tobacco consumption can be enormous on the economies of countries.
Furthermore, this study found that, on average, the economic burden attributable to tobacco use accounted for 0.28% of GPD between 2013–2020 in Nigeria, which is a significant amount considering the fiscal constraints as well as the economic challenges faced in the country in recent years. This finding is corroborated by a systematic review which found the direct and indirect economic costs of tobacco use accounted for about 1.5%–6.8% of health expenditure nationally and was responsible for approximately 0.22%–0.88% of the GDP of countries34. Also, a similar study conducted in India reported that tobacco use was about 1.04% of the total GDP of the country23.
Strengths and limitations
This study has some limitations in that the all-cause relative risk of morbidity and mortality used for the estimates was that reported from another country. Even though this represented the best approach for this study, the estimates in the study will have benefitted from country specific values in terms of the all-cause relative risk of morbidity and mortality due to tobacco consumption. On the other hand, the study’s strength was that it provided estimates of the economic burden of tobacco consumption in Nigeria spanning several recent years. As such, this study reported valuable information for policy makers in assessing the economic efficiency of public health investments towards controlling tobacco use in Nigeria.
Implications
In Nigeria, there are about 11 million tobacco smokers. Although earlier studies used a micro-economic approach, this study adopted a more comprehensive approach (a macroeconomic perspective) by using aggregate expenditure categories related to non-communicable diseases as well as the resulting morbidity and mortality to calculate the economic cost of tobacco use in Nigeria. Between 2013 and 2020, tobacco use imposed about 0.28% economic burden on the country’s GDP, or almost $9.45 billion. So, lowering the level of tobacco use will free funds that can be used to support other crucial sectors of the Nigerian economy.
CONCLUSIONS
Considering the enormous economic burden of tobacco use that is evident in this study, the Nigerian economy as well as public and population health will benefit from intensifying efforts to fully adopt ‘best buys’ policy recommendations to control tobacco use in the country. The findings in this study provide the needed information for galvanizing public health investments to prevent and control the effects of tobacco use on health as well as its impact on the economy. Specific policies that have been proven to be effective in controlling tobacco consumption globally include the use of economic tools (through a regular increase in excise taxes) and the use of legislative tools as strategies for curtailing the increase in tobacco use.