INTRODUCTION
The first case of the novel Coronavirus disease (COVID-19) was reported in Wuhan, China, during the fall of 20191. By 11 March 2020, COVID-19 was declared a pandemic by the World Health Organization (WHO) after more than 100000 individuals had been infected with SARS-CoV-22. Nigeria reported the first case of COVID-19 on 27 February 2020 and had recorded less than 1000 COVID-19 cases by 31 March 20202,3. Due to the highly infectious nature of COVID-19, many countries instituted lockdown measures to curtail its spread3,4. In Nigeria, some hospitals initially suspended operations to reduce staff exposure to the public5. Paradoxically, patients also minimized their hospital visits to avoid contact with the hospital staff, whom they considered high-risk and other infected patients. As a result, managing various ailments and diseases like hypertension, diabetes mellitus, and malaria were challenging to carry out.
Nearly one-half of the world population lives in malariaendemic countries6. Malaria is one of the life-threatening diseases endemic to Africa. Out of every ten malaria deaths, 9 occur in Sub-Saharan Africa, reportedly more among pregnant women and children aged <5 years7. The economic loss due to malaria in Africa is estimated at more than 2 billion US dollars annually. It is known that poverty exacerbates the malaria situation, and malaria contributes to the poverty of the region. Thus, it is believed that malaria is directly responsible for a growing deficit of up to 1.3% per year in some African countries7. The yearly economic loss due to malaria in Nigeria has been placed at 132 billion NGN (1000 Nigerian Naira about US$2.4) in terms of treatment costs, prevention, and loss of man-hours8.
Various malaria intervention programs were introduced by the government and its partners in order to reduce its scourge and eliminate malaria in Africa9. Key among them is the rollback malaria (RBM) initiative that was signed in Dakar, Senegal, in 1998 by various multilateral organizations, including the United Nations Children’s Fund, WHO, and the African Union8. It recommends the use of long-lasting insecticide-treated nets (ITNs), intermittent preventive therapy and case management, as part of the measures to reduce the burden of malaria in vulnerable communities, particularly among pregnant women and children below five years of age9. The RBM program was launched in Nigeria in 2000 and resulted in a 30% decline in malaria incidence between 2001 and 20138. Data from the Nigeria Demographic Health Survey 2018, reported that malaria prevalence among children <5 years has decreased from 42% in 2013 to 23% in 2018. Malaria testing is cost-intensive in Nigeria, both in public and private healthcare facilities10. Malaria treatment-seeking behavior is generally poor in Nigeria, with a large proportion practicing self-medication.
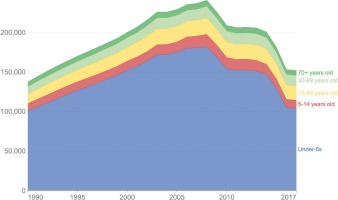
In their research on the indirect effects of the COVID-19 pandemic on malaria intervention coverage in Africa, Weiss et al.11 stated that the disruption to malarial intervention during the COVID-19 lockdown could almost double malaria mortality in 2020 and potentially lead to higher mortality rates in subsequent years. Malaria-related deaths frequently occur in Nigeria (Figure 1)12. Seasonality has been implicated in the understanding of malaria cases and deaths, with a higher proportion of malaria cases and deaths reported during the rainy season. Antimalarials have helped to keep malaria cases and deaths at a minimum. If access to antimalarials and malaria treatment gets disrupted, the impact on deaths is significant – up to 100000 additional malaria deaths could occur. Under a scenario of disruptions to essential malaria services, such as reduction in case management, the impact could be profound. Therefore, it is important to assess the impact of the malaria intervention coverage before and during the COVID-19 pandemic13. The findings from this study would help design programs that will help sustain progress made on malaria intervention coverage in the future. This study, therefore, aimed to access the uptake of malaria intervention services in Nigeria before and during the COVID-19 pandemic.
METHODS
Study area
This study utilized the data collected for Nigeria in the COVID-19 Health Services Disruption Survey 202014. The other countries where data were also collected were Benin, Burkina Faso, Côte d'Ivoire, Democratic Republic of the Congo, Ethiopia, Ghana, Kenya, Liberia, Mali, Mozambique, Niger, Rwanda, Senegal, Sierra Leone, Somalia, Tanzania, Uganda, Zambia, and Zimbabwe. Nigeria is the largest country with the most buoyant economy in west Africa, with an estimated population of 206 million15.
Data collection
Data used were extracted from the COVID-19 Health Services Disruption Survey 2020. The period covered in the survey was December 2019 – July 2020. The pre-COVID-19 period was defined as December 2019 – February 2020, while the COVID-19 period was defined as March–July 2020. Information on health services disruption was collected using a questionnaire-based survey which covered both periods. The data were collected throughout July 2020 from members of the public who had access to both smart phones and internet connections using the Premise platform. Premise is a smartphone-based application that provides data collection capabilities throughout the world. The survey was designed by the Institute for Health Metrics and Evaluation (IHME) in collaboration with the Bill and Melinda Gates Foundation and was implemented by Premise. Incoming data were reviewed and validated by Premise and then transferred to IHME, where they underwent further verification and stored in secure databases maintained by IHME14.
The questionnaire had two sections. Section A described sociodemographic characteristics such as age, sex, location, occupation, ethnicity, religion, financial situation, and an average number of persons in the household. In section B, survey questions pertaining to malaria were divided into two periods: before and during the COVID-19 pandemic. Questions for the period before the COVID-19 pandemic included: ‘Were you able to visit healthcare facilities during December – February?’; ‘What was the reason you were not able to visit healthcare facilities during December – February?’; ‘How many times did you visit healthcare facilities during December – February?’; ‘Did you have malaria symptoms during December – February?’; ‘Were you tested for malaria during December – February?’; and ‘What antimalaria medication did you use during December – February?’.
Questions for the COVID-19 pandemic period included: ‘Were you able to visit healthcare facilities since March?’; ‘What was the reason you were not able to visit a healthcare facility since March?’; ‘How many times did you visit a healthcare facility since March?’; ‘Have you had malaria symptoms since March?’; ‘Have you been tested for malaria since March?’; and ‘What antimalaria medication did you use since March?’.
Sampling/population
IHME, Bill and Melinda Gates Foundation, and Premise, determined target quotas for each country prior to data collection. Target quotas were based primarily on the size of the Premise user network in each country. Progress towards target quotas was monitored over the course of data collection. In locations where the number of responses fell significantly below target quotas, then Premise actively promoted the survey through measures such as re-engagement campaigns and targeted advertisements to increase the number of respondents. Weights were not calculated for the malaria disruption survey. Individual data were available for 1986 Nigerians. However, the completeness of the data was 99.9%.
Statistical analysis
The IBM SPSS Statistics for Windows Version 25.0. IBM Corp. 201716 was used. Descriptive statistics were conducted on sociodemographic variables. Bivariate analysis, using chisquared tests, were used to determine the association between malaria preventive practices before and during the COVID-19 pandemic in Nigeria. These included the number of ITNs, presence of malaria symptoms, visits to a healthcare provider, number of visits, and enrolment in malaria tests. The variable ‘Paid visit to healthcare facilities’ was used as an indicator of willingness to seek malaria treatment. The association between paid visit to healthcare facilities and sociodemographic characteristics of respondents was determined using chi-squared tests. Binary logistic regression tests were independently conducted on significant variables at the bivariate level both for before and during the COVID-19 pandemic. The significant variables at the two periods were modelled into two regression analyses: before and during the COVID-19 pandemic. Thus, all the significant variables were controlled for in the logistic regression models. The level of statistical significance was set at p<0.05.
RESULTS
Among the 1985 respondents, 1522 (76.7%) were males, and 960 (48.4%) were aged ≤25 years. Also, 711 (35.8%) lived in the city or metropolitan area, and 1292 (65.1%) had attained graduate/postgraduate educational level. In addition, 733 (36.9%) belonged to the Yoruba ethnic group, 1033 (52.0%) were Christians, and 1115 (56.2%) lived with four or more persons in their households (Table 1).
Table 1
Sociodemographic characteristics of respondents in Malaria Premise survey, 2020
Table 2 shows the characteristics of malaria preventive practices among respondents before (December 2019 – February 2020) and during the COVID-19 pandemic (March–July 2020). Before the COVID-19 pandemic, 338 (28.5%) had three or more ITNs, and during the COVID-19 pandemic 286 (34.7%) had three or more ITNs (χ2=8.36, p=0.004). Before the COVID-19 pandemic, 1104 (55.6%) had malarial symptoms, and during the COVID-19 pandemic 881 (44.4%) had malarial symptoms (χ2=42.759, p≤0.001). Before the COVID-19 pandemic, 927 (84.0%) had paid a visit to healthcare providers, and during the COVID-19 pandemic, 708 (79.3%) had paid a visit to healthcare providers (χ2=6.99, p=0.008). Furthermore, 482 (70.8%) tested positive for malaria before the COVID-19 pandemic, while 313 (62.6%) tested positive for malaria during the COVID-19 pandemic (χ2=8.40, p=0.004).
Table 2
Characteristics of malarial preventive practices among respondents before and during the COVID-19 pandemic among the Nigerian population, 2020
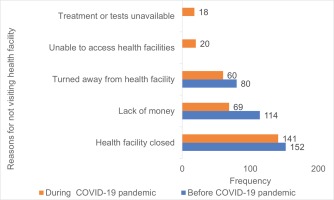
Figure 2 describes the self-reported reasons for respondents’ failure to visit a healthcare provider for malaria diagnosis and testing before and during the COVID-19 pandemic. Due to the closure of health facilities, 152 (28.2%) did not visit health providers before the COVID-19 pandemic, while 141 (32.3%) did not visit health providers during the COVID-19 pandemic. During the COVID-19 pandemic, 20 (4.6%) did not visit health providers because they were unable to access health facilities due to lockdown restrictions. On the other hand, 18 (4.1%) attributed their failure to visit health providers due to the unavailability of test for malaria during the COVID-19 pandemic.
Figure 2
Self-reported reasons for failure to visit a healthcare provider for malaria diagnosis and testing before and during the COVID-19 pandemic, 2020
The frequently used medications for the treatment of malaria before the COVID-19 pandemic included Amodiaquine, Artemisinin Combination therapy, Chloroquine, Fansidar, Artesunate injection, and Primaquine, during the COVID-19 pandemic they also included Artesunate rectal pills. Among the 6 (1.2%) persons who did not use medications for malarial treatment before the COVID-19 pandemic, 3 (50.0%) stated their unwillingness to use medications, 2 (33.3%) did not use medications due to the side effects, and 1 (16.7%) did not use medications due to the lack of money. Among the 10 (3.2%) who did not use antimalarial medications during the COVID-19 pandemic, 3 (30.0%) stated their unwillingness to use medications, and 3 (30.0%) did not use medications due to financial constraints. In addition, 2 (20.0%) did not use medications due to the fear of side effects, and 2 (20.0%) did not use medications due to the unavailability of medicines at the health facility.
Before the COVID-19 pandemic, 485 (50.5%) people aged ≤25 years visited healthcare facilities compared to 348 (41.5%) aged 26–35 years, and 94 (50.5%) persons aged ≥35 years (χ2=15.93, p≤0.001). Also, 593 (45.9%) individuals with graduate/postgraduate education paid visits to healthcare facilities compared to 18 (72.0%) with primary or lower education, and 310 (48.3%) with secondary/technical/high school education (χ2=7.33, p=0.026) (Table 3).
Table 3
Association between sociodemographic characteristics and visit to healthcare provider before and during COVID-19 pandemic, 2020
During the COVID-19 pandemic, 385 (39.9%) persons aged ≤25 years visited healthcare facilities compared to 260 (31.0%) aged 26–35 years, and 64 (34.9%) aged >35 years (χ2=15.53, p≤0.001). Also, 445 (44.4%) with graduate/postgraduate education visited healthcare facilities compared to 18 (72.0%) with primary education, and 243 (37.9%) with secondary/technical/high school (χ2=16.37, p≤0.001) (Table 3).
Before the COVID-19 pandemic, individuals aged 26–35 years had 21% less odds of paying visits to healthcare facilities compared to those aged ≤25 years (AOR=0.79; 95% CI: 0.65–0.97, p=0.021). However, those aged >35 years had more odds of paying visits to healthcare facilities compared to those aged ≤25 years (AOR=1.06; 95% CI: 0.77–1.46, p=0.732). Also, those with primary or lower education level had nearly three times the odds of visiting healthcare facilities compared to those with graduate/postgraduate education (AOR=2.54; 95% CI: 1.04–6.20, p=0.041) (Table 4).
Table 4
Determinants of visits to healthcare facilities for management of malaria before and during the COVID-19 pandemic among the Nigerian population, 2020
| Variables* | AOR | 95% CI | p | |
|---|---|---|---|---|
| Lower | Upper | |||
| Paid visit to healthcare facilities before COVID-19 pandemic | ||||
| Age (years) | ||||
| ≤25 | 1 | |||
| 26–35 | 0.793 | 0.650 | 0.966 | 0.021 |
| >35 | 1.058 | 0.765 | 1.463 | 0.732 |
| Location | ||||
| City center or metropolitan area | 0.570 | 0.460 | 0.705 | <0.001 |
| Suburban/peri-urban | 1.146 | 0.911 | 1.441 | 0.243 |
| Rural | 1 | |||
| Education level | ||||
| Primary or lower | 2.539 | 1.040 | 6.197 | 0.041 |
| Secondary/technical/high school | 1.022 | 0.837 | 1.248 | 0.831 |
| Graduate/postgraduate | 1 | |||
| Paid visit to healthcare facilities during COVID-19 pandemic | ||||
| Sex | ||||
| Male | 1.219 | 0.967 | 1.538 | 0.094 |
| Female | 1 | |||
| Age (years) | ||||
| ≤25 | 1 | |||
| 26-35 | 0.770 | 0.625 | 0.947 | 0.013 |
| >35 | 0.848 | 0.603 | 1.192 | 0.343 |
| Location | ||||
| City center or metropolitan area | 0.510 | 0.400 | 0.651 | <0.001 |
| Suburban/peri-urban | 0.844 | 0.668 | 1.066 | 0.155 |
| Rural | 1 | |||
| Education level | ||||
| Primary or lower | 3.841 | 1.560 | 9.454 | 0.003 |
| Secondary/technical/high school | 1.041 | 0.845 | 1.282 | 0.709 |
| Graduate/postgraduate | 1 | |||
During the COVID-19 pandemic, individuals aged 26–35 years had 23% fewer odds of paying visits to healthcare facilities compared to those aged ≤25 years (AOR=0.77; 95% CI: 0.63–0.95, p=0.013). Individuals aged >35 years had nearly 15% fewer odds of paying visits to healthcare facilities compared to those aged ≤25 years (AOR=0.85; 95% CI: 0.60–1.19, p=0.343). Also, individuals with primary or lower education level had nearly four times the odds of paying visits to healthcare facilities compared to those with graduate/postgraduate education (AOR=3.84; 95% CI: 1.56–9.45, p=0.003) (Table 4).
DISCUSSION
This study found that more households used ITNs during the COVID-19 pandemic compared to the period before the pandemic. The endemicity of malaria in Nigeria and public health campaigns on the use of ITNs as malarial preventive measures17 could provide some explanation for this. In a bid to reduce the risk of contracting COVID-19 in hospital settings, many individuals could have been encouraged to adopt the use of ITNs as a malaria preventive strategy. The COVID-19 pandemic made a lot of people aware of their health and placed a premium on it. COVID-19 information generally exposed them to more health education via the various traditional and social media, because they spent more time at home. Findings from this study revealed that fewer people had symptoms of malaria during the COVID pandemic than the period before the COVID-19 pandemic. There is a possibility that some malarial symptoms were ascribed to COVID-19 due to the similarities between the two infections. Cameroon et al.18 reported a significant intricate relationship between COVID-19 and malaria cases.
It is known that the major drivers of infectious diseases, including COVID-19, are economic collapse and health system failure. Findings from studies conducted in Venezuela, Brazil, and Colombia, reveal that nearly 90% of total malaria cases are attributed to recent migration19. The COVID-19 pandemic caused a substantial economic impact globally, thus causing malaria resurgence in these regions, although its extent has not been adequately documented.
Also, there was a noticeable decline in visits to health providers before COVID-19 compared to during the pandemic. The major reason given was the closure of health facilities. An underlying explanation for the closure of health facilities in Nigeria is the many episodes of industrial action embarked on by healthcare workers. Poor healthcare leadership and management have been identified as some of the most common causes of industrial action among healthcare workers, regardless of the cadre20. Closure of health facilities during the COVID-19 pandemic was adopted as one of the proven public health safety measures required to break the chain of COVID-19 transmission21. It was, therefore, likely that sick people either patronized patent and proprietary medicine vendors or practiced self-medication22-24. Rogerson et al.25 also stated similar reasons that individuals stopped attending health facilities due to fear of exposure to COVID-19 or financial constraints, and healthcare workers required additional resources to protect themselves from COVID-1925. Black et al.25,26 noted that healthcare staff shortages due to COVID-19 illness could have discouraged people from hospital consultations.
Findings from this study revealed that young people (aged <25 years) had higher odds of visiting health facilities for the management of malaria both before and during the COVID-19 pandemic. This finding elucidates that younger people are more health literate regarding the standard index of prompt malaria detection and commencement of management. Evidence from literature reports that malaria symptoms such as fever recede with increasing age27,28. Thus, younger people are more likely to develop these symptoms and seek prompt case management options. To improve visits to healthcare facilities when malaria infection is suspected among older people, invigoration of public health campaigns on the need for diagnostic treatment is required. An interesting factor to explore is that health decisions, such as paying visit to health facilities for case management of malaria, are often taken by older persons, who are responsible for the welfare of younger persons.
In the period before and during the COVID-19 pandemic, those with lower education level had a higher likelihood of visiting healthcare facilities to seek malaria management compared with those with higher education levels. Thus, it could be inferred that educated persons are more likely to practice self-medication once they develop malaria symptoms. In addition, individuals with low level of education have good health literacy regarding the adequate management of malaria in healthcare facilities. Therefore, strategies for improving malaria-related health literacy among highly educated persons should be considered. For instance, awareness campaigns should be tailored towards educated persons. Active engagement of the modern media platforms, such as WhatsApp, Instagram, and Twitter should be undertaken.
During the COVID-19 pandemic, males were found to have a higher likelihood for healthcare visits for management of malaria. This elucidates that women are less likely to visit the hospital for malaria care. Evidence from the Nigeria Demographic Health Survey reports that 52% of women sleep under ITNs. This could therefore indicate that females adopt malaria preventive practices, such as sleeping under ITNs, more compared to males29. Thus, more males are likely to be infected with malaria and visit healthcare facilities to seek care. The use of ITNs among all members of the population, especially men, should be promoted.
From this study, we identified that individuals who lived in suburban or rural areas were more likely to visit healthcare facilities for malaria management compared to those in urban areas. This finding could be due to the presence of socioeconomic and housing factors such as good income (above the national minimum wage), furnished wall, and the absence of orifices that are protective against malaria in urban areas. As a result, residents of urban areas are less likely to develop malaria. However, evidence from literature indicates that many urban communities observe poor sanitation practices30. Poor sanitation and drainage practices have been identified as risk factors for malaria in urban areas30. The societal hustle and bustle in urban settings and the need to meet financial demands, therefore could dissuade many urban residents from paying visits to healthcare facilities when malaria infection is suspected. To promote healthy societies in urban settings and avoid economic losses associated with severe malaria, the Ministry of Health at national and state levels should liaise with labor organizations to include malaria awareness programs in their schedule at regular intervals.
It is noteworthy that more people enrolled for malaria tests before than during the pandemic, even though it was not statistically significant. Generally, it is uncommon for people in Nigeria to run malaria tests as they will rather treat it with antimalarial medications when they suspect some symptoms than enroll for tests. This finding could be attributed to the fear of exposure to healthcare workers since many healthcare workers were confirmed COVID-19 positive cases. Of the population sampled, there were more positive malaria results before the COVID-19 pandemic than during the COVID-19 pandemic. This could result from the similarities between COVID-19 and malaria symptoms as established from the literature26,27. Although malaria is endemic in Nigeria, the close similarities between malaria and COVID-19 symptoms caused confusion among many. Furthermore, the novelty of COVID-19 and lack of sufficient knowledge about it promoted public skepticism regarding its existence. The Federal Ministry of Health and the Nigeria Centre for Disease Control, under the auspices of the Africa Centre for Disease Control, sponsored many health campaigns to debunk fallacies and myths related to COVID-1922,23. Yet, many individuals entertained misconceptions on COVID-19. To this end, many individuals in Nigeria who eventually tested positive for COVID-19 could have initially thought they had malaria. As a result, malarial treatment could have commenced before COVID-19 screening was considered22,23. Likewise, they may have used artemisinin-combination therapies (ACTs) over the counter. Irrational use of ACTs could hinder the effectiveness of antimalarial medications and cause antimalarial resistance. For this cause, antimalarial stewardship interventions aimed at promoting rational use of antimalarials only when prescribed by a skilled health professional need to be promoted.
COVID-19 testing is often considered as a last resort for many people following the persistence of symptoms such as anosmia (inability to smell) or the development of complications, such as breathing difficulties. Data from clinical and virological studies have reported that the shedding of SARS-CoV-2, the causative organism for COVID-19, is highest in the first three days of infection. During this period, the viremia level is at its peak. Given the effectiveness of antimalarials in the clinical management of COVID-19 cases, the use of antimalarials could lead to a significant reduction in the virus load before COVID-19 tests are conducted24. Thus, many COVID-19 tests may yield negative results since the period of high infectiousness has been bypassed.
Strengths and limitations
The absence of weights in the calculation of the sample size limits the generalizability of the study. Details such as exact population group, and geographical distribution of respondents were not adequately captured in the original data. Despite these limitations, this study provided knowledge on the differences in the uptake of malarial intervention programs before and during the COVID-19 pandemic. We also reported the factors responsible for the observed results during the COVID-19 pandemic.
CONCLUSIONS
The COVID-19 pandemic had a negative impact on some components of malaria intervention coverage in Nigeria, namely malarial testing and visits to health facilities for malarial treatment. To ensure a steady decline in the malaria disease burden, malarial intervention coverage programs, such as antimalarial stewardship should be promoted. This would include the provision of rapid diagnostic kits for community pharmacists. These kits would enable the prompt diagnosis of malarial infection by detecting malaria antigens in the blood. Furthermore, malaria diagnosis should be linked with COVID-19 screening and testing of suspected or confirmed COVID-19 cases to avoid misdiagnosis and enable easy management. Because fever is a common symptom in both diseases, this study emphasizes the need to educate healthcare providers and individuals about the possibility for misdiagnosis of malaria for COVID-19, including the co-existence of the two infections. More and regular ITNs distributions are needed to ensure the prevention of malaria. Improved healthcare leadership and management should be prioritized to reduce health services disruption in Nigeria in a bid to promote population health. These would help to preserve the gains already made from previous malaria programs.