INTRODUCTION
Secondhand smoke (SHS) refers to either smoke from burning tobacco products (sidestream smoke) or that exhaled by smokers (exhaled mainstream smoke)1,2. Exposure to secondhand tobacco smoke (SHS) is an important public health problem worldwide3–5, with one-third of adults reported to be regularly exposed to it worldwide4. This problem is serious among children and adolescent nonsmokers5,6. Worldwide, it was estimated about a decade ago that SHS exposure kills over 0.6 million people each year4,7. Moreover, with the increased prevalence in tobacco smoking reported, especially in Low and Middle-Income Countries (LMICs) such as Nigeria, the number of people that die yearly from exposure to SHS may have increased substantially.
Exposure to SHS has been found to have several illhealth effects on those exposed, especially the children and adolescents. These include mental health disorders, atherosclerosis, kidney problems, upper and lower acute respiratory tract infections, acute and chronic ear infections, exacerbation of asthma, and adverse growth outcomes in children8–13. Other reported health hazards are: bladder cancer, increased lead in the bloodstream, cognitive impairment and poor academic performance14–16. Reported oral effects include pigmentation of the gums, periodontitis, caries, tooth loss and orofacial cleft17–21. Exposure to SHS is also significantly associated with the uptake of tobacco smoking habit during the adolescent stage of growth6,22,23, a development which is posing a public health problem.
Though the law restricting smoking in public spaces has led to significantly reduced exposure to SHS4, the overall prevalence of exposure to SHS is still high even in countries that have banned smoking in public places5. Factors reported to be associated with a high risk of exposure to SHS among adolescents are: having a smoking friend or smoking family member, inadequate knowledge about the harmful effects of tobacco smoke, poor attitude towards tobacco smoking, and ban of tobacco use in public places5,22,24,25.
There is a paucity of research on the burden of exposure to SHS among adolescents in Nigeria. The last survey among school-going adolescents using GYTS was conducted in 2008, and a high prevalence of exposure to SHS among schoolgoing adolescents was reported, though varied across the five cities where the survey was conducted. The prevalence of both home and public (outside home) exposure to SHS was lowest in Ibadan at 14.5% and 25%, respectively, while home exposure was highest in Calabar (31.3%) and public exposure was highest in Kano (55.8%)26. However, a recent study27 on outdoor (motor-parks, roadsides and street corners) tobacco smoking conducted in Ibadan city revealed a prevalence of 63.8%. With such values in the prevalence of tobacco smoking in open spaces, it becomes important to document the SHS exposure level in Ibadan, especially among non-smoking adolescents. Such information has the potential to highlight specific areas for intervention in both oral and general health promotion and disease prevention among the adolescents and youths.
A proper understanding of the severity of the exposure to SHS among adolescents and its associated factors will facilitate the development of an effective intervention to curtail it. Thus, this study aimed at estimating the current prevalence and determinants of exposure to SHS both at home and outside home, among non-tobacco smoking adolescents who were enrolled in schools in the Ibadan metropolis, Nigeria.
METHODS
Study design
A descriptive cross-sectional study was conducted in Ibadan metropolis, Oyo State, Nigeria. The metropolitan part of the city of Ibadan has five Local Government Areas (LGAs). The typical secondary schools have six class levels (Junior and Senior secondary schools, 1–3).
Study population and selection of study participants
The study was carried out among adolescents who were enrolled in both public and private secondary schools, irrespective of their smoking status. Only adolescents between the ages of 10 and 19 years and who had completed at least one year in the school were included in the study. Consequently, the students in the Junior Secondary School 1 (JSS1) classes were excluded.
Multistage sampling technique was used in selecting the study participants. Three LGAs out of the Five LGAs were randomly selected from the study area. A list of all the secondary schools (public and private) in each of the selected LGAs was obtained from the Ministry of Education, Oyo State. From the list, six secondary schools (three public and three private) were selected in each of the three LGAs using simple random sampling method, making a total of 18 schools. Finally, from each of the selected schools, 10 students were selected per class: Junior Secondary School 2 to Senior Secondary School 3 (JSS2 to SSS3) using stratified sampling method.
Data collection procedure
A self-administered semi-structured questionnaire was used for data collection. The questionnaire was adapted from the standardized questionnaire for Global Youth Tobacco Survey (GYTS)28 and literature29,30. Of the total of 900 selected study participants, 39 declined participation in the research. These were mainly the SSS 3 students, who attributed their nonparticipation to the fast-approaching Senior Secondary School Leaving Certificate Examinations. Thus, the total number of respondents was 861. Ethical approval (UI/ EC/18/0243) was obtained from the University of Ibadan/University College Hospital Ethics Review Board before the commencement of the study. Permission was obtained from both the Ministry of Education, Oyo State and the school principals of the selected secondary schools. Consent and assent were obtained from the parents/guardians and the students, respectively, before the conduct of the study. The respondents were assured of the confidentiality and anonymity of the information they provided.
Study measures
The outcome variable is exposure to SHS. This outcome was further categorized based on the location where the exposure occurred. These included exposure: inside home, outside home, both inside and outside home, and either inside or outside home. Exposure to SHS inside and/or outside the home was determined based on the answer to the questions: ‘During the past 7 days, on how many days has anyone smoked inside your home, in your presence?’ and ‘During the past 7 days, on how many days has anyone smoked in your presence, at a public place, other than your home?’5,24,31–34. A respondent’s status to SHS exposure whether inside and/ or outside home was determined to be negative only if a ‘0 days’ option was selected; otherwise, he/she was classified as exposed. As with similar studies, the responses of the participants were used to determine respondents who were exposed ‘both inside home and outside home’ by combining only those that responded positively to both ‘SHS exposure at home’ and ‘SHS exposure outside home’24,32–34. Exposure to ‘either inside or outside home’ was ascertained from participants that answered positively to either ‘SHS exposure at home’ or ‘SHS exposure outside home’35.
Smoking status of the participants was determined using the questions: ‘Have you ever smoked cigarette, even if it is one or two puffs?’ and ‘During the past 30 days, on how many days did you smoke cigarettes?’. Those who responded negatively to the two questions were classified as ‘never smokers’ and ‘non-current smokers’, respectively; they constituted the study population for this study (never/non-current smokers).
The social class of the participants was determined based on the classification by Oyedeji et al.36. Different scores were allocated to the educational level and occupation of the respondents’ parents/guardians, and the average score per participant was calculated. Following this, the respondents were further categorized into low, middle or high social class based on their scores36. Perception about the adverse effect of tobacco smoking and the exposure to SHS was assessed by the question: ‘Do you think the smoke from other people’s tobacco smoking is harmful to you?’ and ‘Do you think smoking tobacco is harmful to your health?’. The options were: ‘Definitely not’, ‘Probably not’, ‘Probably yes’, and ‘Definitely yes’. The first two options were later merged into ‘no’ and the last two options combined as ‘yes’. Another independent variable was the adolescents’ participation in tobacco errands, which was assessed by asking: ‘Do the elder ones in your household and community send you on errands to buy tobacco/cigarettes?’ with ‘yes’ and ‘no’ as the options.
Statistical analysis
The data were analyzed using Statistical Package for Social Sciences (SPSS) version 25. Only the data of respondents with the characteristic of interest (non-current smokers) were analyzed. Descriptive analysis of the continuous variables are presented as means with standard deviation, while categorical variables, such as the sociodemographic and the outcome variables, are presented as proportions. Associations between the outcome variables (exposure to SHS at different locations) and the independent variables such as age, gender, smoking status of parents and of close friends, attitude towards smoking and knowledge about harmful effects of smoking and exposure to tobacco smoke were based on chisquared test. Multiple logistic regression model was used to estimate the relationship between the independent variables and exposure to SHS. The adjusted odds ratios (AOR) and 95% confidence intervals (95% CI) are reported. All statistical inferences are based on 5% significance level.
RESULTS
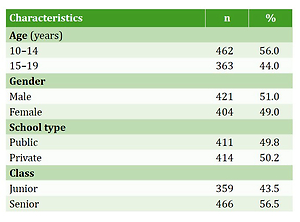
The total number of respondents who were either never smokers or non-smokers was 825, with a mean age of 14 (SD=1.72) years, of which 421 (51.0%) were males (Table 1). About half (49.5%) of the respondents belonged to a high social class, and 464 (56.2%) were of the opinion that the majority of their peers smoked tobacco (Table 1). About 10.2% and 12.2% of the adolescents had close friends and family members who smoke, respectively, while 56 (6.8%) of the respondents ran errands to buy tobacco products for adults (Table 1).
Table 1
Sociodemographic characteristics and prevalence estimates of predictors of exposure to secondhand tobacco smoke (SHS) among non-smoking, in-school adolescents in Ibadan, Nigeria, 2018 (N=825)
Exposure to SHS
The prevalence of exposure to SHS ‘inside home’, ‘outside home’, ‘both inside and outside home’ and ‘either inside or outside home’ were 6.1%, 31.5%, 5.1%, and 32.5%, respectively (Table 2). Even though only 6.1% were exposed at home, most (84.0%) were also exposed to SHS outside their homes. On bivariate analysis, factors such as the school type, house type, social class, having a smoking friend and smoking family, and going on errands to buy tobacco products, were significantly associated (p<0.05) with all the four forms of exposure to SHS (Table 3). However, following the logistic regression analysis, the following factors were predictors of exposure to SHS: having a family member who smokes (AOR=4.56; 95% CI: 2.36–8.80) and going on errands to buy tobacco products (AOR=3.11; 95% CI: 1.40–6.91) were found to be independently associated with exposure to SHS at home. Similar factors were also associated with the exposure to SHS, both inside and outside home (Table 4). As for exposure to SHS outside home, those who had smoking family members (AOR=1.75; 95% CI: 1.10–2.76) or friends (AOR=2.62; 95% CI: 1.58–4.35), who were sent on errands to buy tobacco products (AOR=3.59; 95% CI: 1.93–6.65), and respondents who believed most of their peers smoke (AOR=1.48; 95% CI: 1.07–2.05) were significantly associated with increased odds of SHS exposure outside home (Table 4). The predictors of exposure to SHS inside or outside home included all the factors that were significantly associated with exposure outside home, as well as belonging to a low social class (OR=1.66; 95% CI: 1.05–2.62; p=0.03) (Table 4).
Table 2
Percentage distribution of exposure to secondhand tobacco smoke (SHS) among non-smoking, school-going adolescents in Ibadan, 2018 (N=825)
| Exposure to SHS | n | % |
|---|---|---|
| Inside home | ||
| No | 775 | 93.9 |
| Yes | 50 | 6.1 |
| Outside home | ||
| No | 565 | 68.5 |
| Yes | 260 | 31.5 |
| Both inside and outside home | ||
| No | 783 | 94.9 |
| Yes | 42 | 5.1 |
| Either inside or outside home | ||
| No | 557 | 67.5 |
| Yes | 268 | 32.5 |
Table 3
Factors associated with exposure to secondhand tobacco smoke (SHS) among in-school adolescents in Ibadan, Nigeria, 2018
| Characteristics | Exposure to SHS | |||||||
|---|---|---|---|---|---|---|---|---|
| Inside home 50 (6.1%) | Outside home 260 (31.5%) | Both inside and outside home 42 (5.1%) | Either inside or outside home 268 (32.5%) | |||||
| n (%) | p | n (%) | p | n (%) | p | n (%) | p | |
| Age (years) | 0.557 | 0.005a | 0.421 | 0.007a | ||||
| 10–14 | 26 (5.6) | 127 (27.5) | 21 (4.5) | 132 (28.6) | ||||
| 15–19 | 24 (6.6) | 133 (36.6) | 21 (5.8) | 136 (37.5) | ||||
| School type | 0.003a | 0.004a | 0.004a | 0.002a | ||||
| Public | 35 (8.5) | 149 (36.3) | 30 (7.3) | 154 (37.5) | ||||
| Private | 15 (3.6) | 111 (26.8) | 12 (2.9) | 114 (27.5) | ||||
| Parents living together | 0.015a | 0.133 | 0.056 | 0.066 | ||||
| 0.031b,a | 0.081b | |||||||
| No | 9 (12.7) | 28 (39.4) | 7 (9.9) | 30 (42.3) | ||||
| Yes | 41 (5.4) | 232 (30.8) | 35 (4.6) | 238 (31.6) | ||||
| House type | 0.001a | 0.018a | <0.001a | 0.031a | ||||
| One room apartment | 7 (12.7) | 25 (45.5) | 7 (12.7) | 25 (45.5) | ||||
| Two rooms | 15 (11.2) | 49 (36.6) | 14 (10.4) | 50 (37.3) | ||||
| Three rooms or more | 28 (4.4) | 186 (29.2) | 21 (3.3) | 193 (30.3) | ||||
| Social class | 0.004a | 0.004a | 0.038a | 0.001a | ||||
| Low | 18 (10.8) | 65 (39.2) | 13 (7.8) | 70 (42.2) | ||||
| Middle | 17 (6.8) | 87 (34.8) | 16 (6.4) | 88 (35.2) | ||||
| High | 15 (3.7) | 107 (26.2) | 13 (3.2) | 109 (26.7) | ||||
| Most of my peers smoke | 0.084 | <0.001a | 0.086 | <0.001a | ||||
| I believe this | 34 (7.3) | 174 (37.5) | 29 (6.3) | 179 (38.6) | ||||
| I don`t believe this/not sure | 16 (4.4) | 86 (23.8) | 13 (3.6) | 89 (24.7) | ||||
| Have a smoking friend | 0.004a | <0.001a | 0.003a | <0.001a | ||||
| No | 39 (5.3) | 211 (28.5) | 32 (4.3) | 218 (29.4) | ||||
| Yes | 11 (13.1) | 49 (58.3) | 10 (11.9) | 50 (59.5) | ||||
| Have a smoking family member | <0.001a | <0.001a | <0.001a | <0.001a | ||||
| No | 30 (4.1) | 211 (29.1) | 26 (3.6) | 215 (29.7) | ||||
| Yes | 20 (19.8) | 49 (48.5) | 16 (15.8) | 53 (52.5) | ||||
| Send on tobacco errands | <0.001a | <0.001a | <0.001a | <0.001a | ||||
| Yes | 12 (21.4) | 38 (67.9) | 12 (21.4) | 38 (67.9) | ||||
| No | 38 (4.9) | 222 (28.9) | 30 (3.9) | 230 (29.9) | ||||
| Can one purchase tobacco near my school | 0.928 | 0.019a | 0.818 | 0.030a | ||||
| 1.000b | 0.743b | |||||||
| No/not sure | 47 (6.1) | 236 (30.5) | 39 (5.0) | 244 (31.6) | ||||
| Yes | 3 (5.8) | 24 (46.2) | 3 (5.8) | 24 (46.2) | ||||
Table 4
Predictors of exposure to secondhand tobacco smoke (SHS) among in-school adolescents in Ibadan, Nigeria, 2018
| Variables | Exposure to SHS | |||
|---|---|---|---|---|
| Inside home | Outside home | Both inside and outside home | Either inside or outside home | |
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| Have a smoking family | ||||
| Yes | 4.56 (2.36–8.80) | 1.75 (1.10–2.76) | 3.59 (1.76–7.33) | 2.08 (1.32–3.28) |
| No (Ref.) | 1.00 | 1.00 | 1.00 | 1.00 |
| Sent on tobacco errands | ||||
| Yes | 3.11 (1.40–6.91) | 3.59 (1.93–6.65) | 3.95 (1.75–8.90) | 3.32 (1.79–6.17) |
| No (Ref.) | 1.00 | 1.00 | 1.00 | 1.00 |
| Have a smoking friend | ||||
| Yes | 2.62 (1.58–4.35) | 2.62 (1.58–4.37) | ||
| No (Ref.) | 1.00 | 1.00 | ||
| Most of my peers smoke | ||||
| I believe this | 1.48 (1.07–2.05) | 1.48 (1.07–2.05) | ||
| I don’t believ/not sure (Ref.) | 1.00 | 1.00 | ||
| Social class | ||||
| Low | 1.66 (1.05–2.62) | |||
| Middle | 1.33 (0.89–1.97)a | |||
| High (Ref.) | 1.00 | |||
Perception of harm from passive and active tobacco smoking
One in every five of the non-smoking adolescents did not believe that exposure to SHS is harmful, and 12.4% disagreed that tobacco smoking is harmful to their health (Table 1). Overall, the study shows that non-smoking adolescents who had a better knowledge of the harm from exposure to tobacco smoke and tobacco smoking itself, were more exposed to SHS across all the locations.
DISCUSSION
We found that about one in every three participants was exposed to tobacco smoke either inside or outside home, the associated factors were: having a smoking family member or smoking friend, running tobacco errands, believing that most of their peers smoke, and belonging to the lowest social class. The prevalence of exposure to SHS at home (6.1%) was much lower compared to exposure outside the home (31.5%), and this finding is generally in agreement with most other studies conducted in Nigeria26,37, West Africa31,34, Africa25,33,35, and worldwide24,34,38. Having a smoking family member and smoking friend was some of the significant factors found in our study, and this is also consistent with many other studies5,22,24,25,35,39.
Though the prevalence of exposure to SHS at home was small, it is noted that the majority were also exposed to SHS outside their homes. The relatively high prevalence of exposure to SHS by these adolescents points to the fact that while Nigeria may have signed the treaty on the implementation of Article 8 of WHO FCTC framework3, the enforcement is probably lacking. Unlike some states in Nigeria, there is no state legislation banning public smoking in Oyo State. And, even though the National Tobacco Control Act banning public smoking was enacted in 2015, enforcement of this law has been weak in Oyo State and across the country40. Comparing the findings from Nigeria GYTS study26 with our research suggests that while SHS exposure inside the home may have decreased, outside exposure has increased in Ibadan over the last decade. Unlike the previous study in 200826, this study did not include current smokers. Thus, it would have been expected that the prevalence of exposure to SHS outside home should have been further decreased (since smokers are generally the most exposed to SHS), but this was not the case. The probable explanation for this difference could be that the GYTS survey was carried out among adolescents aged 13–15 years, while all adolescents (10–19 years) were included in the current study.
The high prevalence of exposure to SHS is a public health problem considering the numerous adverse effects that such exposure can cause to adolescents. Thus, urgent steps must be taken to reduce this exposure by ensuring that current smokers are encouraged to quit, and non-smokers are encouraged to make the right decision of avoiding exposure to tobacco smoke. The fact that over one-fifth of the respondents were unaware that exposure to SHS is harmful is a cause of concern, and the level of awareness was higher in the private schools than the public schools. Thus, there is a need for more health education concerning tobacco smoking and its ill-health effects, especially with regard to passive smoking.
What is, however, more surprising is that a higher proportion of the respondents with better perception about the ill-health effects of tobacco smoke were still more exposed to SHS. It thus suggests that having a better perception has not translated to a positive behaviour of avoiding passive smoking among this population. While this may be unusual, it is in agreement with the result of the survey conducted among adolescents (13–15 years) in 168 countries34. We are inclined to believe that the strong culture norm of respect for elders in this society (Southwest Nigeria) could have impeded their ability to avoid exposure to SHS from smoking parents/elders. This underscores the importance of implementing smoke-free policies, as well as educating smoking parents/elders on the need to stop smoking, and more importantly, the danger to their children and adolescents. As was reported in a similar study conducted among children in Spain41, social inequality was found to be independently associated with exposure to SHS, either inside or outside home. Adolescents of low social class were found to be about two times more likely to be exposed to SHS compared with those of high social class. This further underscores the need for health promotion in addressing this problem.
Limitations
This study is not without its limitations, being of a crosssectional study design causality cannot be inferred. However, since we did not set out to find causality but instead the factors associated with exposure to SHS, we do not consider this to be a problem. Also, the information provided was self-reported, hence, prone to misreporting. While we agree that this is indeed a challenge, we tried to avoid such by explaining to the participants that the questionnaires were anonymized and their responses cannot be traced back to them. With regard to the risk of recall bias, we do not expect this to be a problem because the information sought was exposure in the recent past (last seven days). However, information gathered will highlight the current situation regarding SHS exposure in Ibadan, since the only available report was obtained in 2008. This study is also likely to stimulate similar studies in other cities across the country so that adequate information will be available to formulate an effective public health intervention for the country.
CONCLUSIONS
The prevalence of exposure to SHS among in-school adolescents in Ibadan, Nigeria, is much higher outside the home than inside the home. Having a smoking family member and smoking friend, going on tobacco-related errands, having the erroneous belief that their peers smoke, and belonging to a low socioeconomic class were the correlates of exposure to SHS. The government must ensure increased compliance with the smoke-free policy. At the same time, tobacco control advocates should intensify efforts in educating adolescents, as well as their smoking relatives and friends about the dangers of active and passive smoking. We encourage further research on the reasons why the perception of harm from exposure to SHS did not translate into avoidance of SHS.